DENTAL DISEASES IN PERSONS WITH SPECIAL NEEDS: PREVENTION STRATEGIES
SHOULD WE THEN IGNORE THEM?
It is critical to prevent dental diseases in these individuals. but, before I continue with prevention strategies, lets look at who a special need person is.
Who is a person with “special needs”?
Special needs are defined as an individual with a mental, emotional, developmental, cognitive or physical disability. An individual with special needs may need help in one or more of the following areas:
- Communication,
- Movement,
- Self-care and
- Decision-making.
For the purpose of this discussion we will consider people with special needs as Persons who have difficulty accessing dental treatment because of the following factors. - Medical,
- Physical,
- Social and
- Psychological
Examples of Special Needs persons
- Attention-Deficit/Hyperactivity Disorder (AD/HD)
- Autism/ Pervasive Developmental Disorder (PDD)
- Blindness/ Visual Impairment
- Cerebral Palsy
- Deaf-Blindness
- Deafness and Hearing Loss
- Developmental Delay (DD)
- Traumatic Brain Injury
- Down Syndrome
- Emotional Disturbance
- Epilepsy
- Intellectual Disability (formerly Mental Retardation)
- Learning Disabilities (LD)
- Severe and/or Multiple Disabilities
- Speech and Language Impairments
- Spina Bifida
- Traumatic Brain Injury
What is the magnitude of the problem?
In the USA 54 million persons (approximate 20% of the population live with one disability). More than 6 million have intellectual disability (about 200 million persons globally). Intellectual disability is more prevalent than blindness or deafness. Many times it is associated with secondary health conditions that place individuals at a greater risk for medical conditions than the general population.
The proportion of persons with sensory, physical and mental disabilities generally increases with age. It can reach 40% for persons 65 years and older.Research has shown that almost two thirds of these persons have difficulty finding a dentist willing to treat them (i.e. in communities where they identify oral health as an important challenge)
In Nigeria there is sparse information available but the common disabilities reported by a researcher in a particular state were visual (37%), movement/physical (32%), hearing (15%) and intellectual and communication problems 16%. The total number of persons living with disability in 2006 was 3,353,169 persons (that is the population of some small countries!!!). Women = 1,544,418 ,Children = 1,002,062 and Men= 806,689.
Dental Problems in special needs patients include
Dental Caries
Periodontal disease
Malocclusion
Gingival hyperplasia
Bruxism
Delayed Eruption
Caries risk
Persons with special health care needs are at increased risk for developing caries for the following reasons:
- Diet
- Xerostomia
- Difficulties performing oral hygiene
- Gastroesophageal Reflux Disease and vomiting
- Gingival hyperplasia and crowding of the teeth
- Medications containing sugar
In persons with special health care needs, uncoordinated chewing may leave more food in the mouth. A weak, uncoordinated tongue may not be able to adequately clean all oral surfaces. Also gagging on the toothbrush, paste, or saliva may inhibit complete brushing of all surfaces. An inability to spit may result in the swallowing of toothpaste.
Tooth eruption
Tooth eruption may be delayed, normal, or advanced in children with special health care needs. Delayed eruption is more common in children with Down’s syndrome and hypothyroidism.
Malocclusion and crowded teeth
Malocclusion and crowded teeth occur more often in children with abnormal muscle tone (cerebral palsy), mental retardation, and craniofacial abnormalities. Crowded teeth are more difficult to clean, thereby increasing the risk of dental caries and periodontal disease.
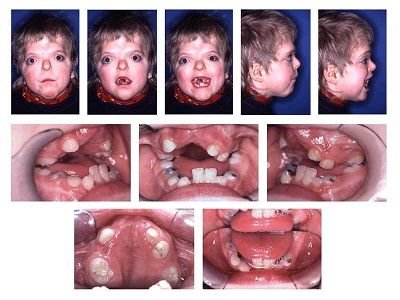
Dental Anomalies
Teeth may vary in shape, size, or number. Dental anomalies are a cosmetic concern and may increase the risk for caries.
Gingival hyperplasia
Gingival hyperplasia usually occurs in children taking anti-epileptic medications for seizures, especially phenytoin. Other medications causing hyperplasia include Calcium channel blockers (e.g nifedipine) and Cyclosporin A.
Chronic gingivitis from poor oral hygiene can also trigger or exacerbate medication induced gingival overgrowth.In addition to the cosmetic concern, gingival hyperplasia puts children at risk for:
- Poor oral hygiene
- Impaired tooth eruption
- Difficulty chewing
- Severe gingivitis
Treatment includes:
Meticulous oral hygiene, discontinuing the offending medication and gingivectomy(cutting off the excess gum) if severe.
Trauma
Trauma to the face and mouth occurs more frequently in children with seizures, developmental delays, poor muscle coordination, and abnormal protective reflexes. Some persons with special needs also exhibit self-injurious behavior, which may damage oral structures.
Bruxism
Bruxism is more common and often more severe in children with cerebral palsy or severe mental retardation. Also occurs in patients who are taking some antipsychotic agents. Bruxism may lead to enamel loss and difficulty with chewing or tooth sensitivity.
Problems with receiving Oral health Care
Persons with special health care needs may not be able to fully cooperate with oral hygiene practices due to gagging, oral defensiveness, or behavioral issues. They may also have difficulty tolerating fluoride liquid, toothpaste, varnish, sealants, or other caries prevention strategies . This is further compounded by the problem of access to care. Problems of accessing care may be due to the followings;
- Limited availability of dentist to treat patients with special health care needs;
- Dentists’ willingness to treat people with special health care needs
- Low awareness of the oral health issues in the patient environment.
- Educational experience and training in treating patients with disabilities or chronic conditions
- The time committed in treatment of Special Need Patient is more.
- Economic factors - Families with Special Need children experience much higher expenditures than required for healthy children especially in situation where there is no insurance coverage.
- Logistic difficulties in receiving the dental care services, due to architectural barriers and public transportation
- Non-financial barriers such as: language – communication problems, psychosocial-oral health beliefs, cultural considerations or norms of caregiver and past dental experience of the caregiver.
- Parental and physician lack of awareness and knowledge may hinder an individual with special need from seeking preventive dental care.
- Other health conditions may seem more important than dental health.
Ideal Prevention Strategies for Special Needs Persons
This should include educating the parents and caregiver on the need for adequate oral health care for these category of patient, control of plaque biofilm with the use of chemical agents such as antimicrobials(e.g Chlorhexidine) and home fluorides, and dietary counselling.
Sealants materials such as glass ionomers that release fluoride, are useful as both preventive and therapeutic approaches in patients with special need and this should be considered for caries control and can only be professionally applied in the dental office. Regular dental visits should be part of the plan to evaluate effectiveness of the program and make modifications when necessary .
The following are basic accepted preventive home care strategies
- Using a fluoridated toothpaste
- Effective plaque removal using a toothbrush and floss
- Using fluoridated water (bottled water if there is no fluoridated community water
- Adopting a healthy diet free of cariogenic sugar
- Regular professional oral health care visits
Behavior change/modification
Dental professionals must realize how difficult it is to change behavior to maintain oral health. Change is effected through education as a major part of any oral hygiene program, whether it is directed at the disabled patient or the caregiver or both. It’s important that the person being taught understands the reasons for good oral health, why any change in behavior is necessary, and the consequences of continuing poor oral hygiene conditions emphasized.
Observe the patient’s or caregiver’s technique directly and if needed make the changes in small increments. If possible, work within what is already being done to minimize the number of changes.Patients should be encouraged to do as much on their own as they are able. Determine the patient’s abilities to understand and follow directions by asking questions during skill assessment.
Learning tools can include use of pictures and/ or modeling of others. The tell–show–do method of teaching may be effective.Each step of the procedure is explained and shown to the patient and then the patient demonstrates the activity.
Design characteristics of self-care tools
Material used for modification should be readily available, lightweight and inexpensive. Device should be easily constructed with replaceable parts (parts that become worn out or dirty should be easily replaced). The device should be easy to use and have minimal set–up time.Toothbrushing
For older patients with limited dexterity, consider the following options:
- An electric or battery-powered toothbrush,
- Extending the brush handle with a tongue depressor,
- Widening the brush handle (wrapping it with a sponge), and
- Using a mouth prop to keep the mouth open during brushing.
Conclusion
The challenges faced by people with special need is enormous so much so that their oral hygiene is often neglected. Parents/Caregivers education is important to ensure that appropriate and regular supervision of daily oral hygiene is maintained.
Dental professionals should develop an individualized oral hygiene program that takes into account the unique disability of the patient. Fluoridated mouth rinse may be applied with the toothbrush.Twice daily brushing with a fluoridated dentifrice should be emphasized to help prevent caries and gingivitis. Toothbrushes can be modified to enable individuals with physical disabilities to brush their own teeth.
Prevention is better than cure!
Prevention is cheaper than cure!
Thank you for reading.
Please note: All images used are from free source.



Thanks for sharing. What are the prescribed dental cares that can be given to babies to achieve well-arranged dental structure?
This is nice and educating. What are the possible side effect of using florinated mouth wash.
Thanks for your comment and question. Fluorinated mouth wash has no serious side effect because the concentration of fluorine in it is low,however excessive fluoridehas devastating effects on the body both local(on the teeth) and systemic(organs and tissues). You will learn more about this in my next post.
Some noobs questions for you.
Do cavities ever get to regrow?
What about teeth that are removed? Any chance of it regrowing?
What is the best toothpaste to prevent cavities that you will recommend for someone in Nigeria?
The second to last picture showed a lot of cavities that were filled, how do people get to have so many holes?
Thanks for sharing.
Thanks for reading and for your questions. Actually for me to be able to do justice to your questions, I think I need to make a post about tooth eruption and cavity formation that will adequately address it all. Meanwhile, let me try and answer some of the issues you raised.
cavity formation involve an interplay between 4 factors : bacterial, susceptible tooth surface, sugar and time. the whole process involves periods of demineralization and remineralization depending on the PH of the saliva at each time. however when demineralization progresses faster than the rate at which remineralization occurs ,cavity formation will occur and it is an irreversible process.so it can never grow back. Also people have a lot of cavity on their teeth because of poor oral hygiene, consumption of lots of refined sugar containing diets. I will explain more in my post .
To the other question, there are two set of dentition that an individual will have in life, primary(milk teeth) and seconday dentition(permanent teeth ). primary @early stage of life and secondary later(after 13yrs). so if it is primary that is removed, the permanent will replace it but if anything happens to the permanet, then no chance of regrowing again.
Any toothpaste that contain fluoride is okay to use .there are so many of them in Nigeria... Close up, Oral B etc.
I hope l have been able to answer your questions, any grey areas will be elucidated more in my next posts. Thank you.
Congratulations @drkomoo! You have completed some achievement on Steemit and have been rewarded with new badge(s) :
Click on any badge to view your own Board of Honor on SteemitBoard.
For more information about SteemitBoard, click here
If you no longer want to receive notifications, reply to this comment with the word
STOPCongratulations @drkomoo! You received a personal award!
Click here to view your Board
Do not miss the last post from @steemitboard:
Congratulations @drkomoo! You received a personal award!
You can view your badges on your Steem Board and compare to others on the Steem Ranking
Vote for @Steemitboard as a witness to get one more award and increased upvotes!