Invasive treatment of cardiac tamponade
The following topic to share is a very complex technique that should only be performed by trained medical personnel, with a high risk of morbidity and mortality but that, in the right hands, improves the quality of life and avoids fatal complications such as death.
From the earliest times, cardiac pathologies have been prominent in both Roman and medical literature. The first writings are from 1649. Riolanus first described pericardial tamponade, then in 1827, Thomas Jowett first described the use of pericardiocentesis as an intervention for pericarditis. Finally, in 1829, Napoleon's surgeon performed the first successful pericardiocentesis.
Pericardiocentesis is a complex technique based on the extraction of fluid from the space located in the pericardium surrounding the heart. This fluid is usually aspirated using a needle and syringe, sometimes requiring the use of a catheter placed in the pericardium or a surgical approach.
This procedure has a double function, both therapeutic and diagnostic, that is, to obtain fluid from the pericardial space and determine its etiology (neoplastic or infectious), to relieve the effusion and therefore the patient's signs and symptoms, or ultimately to improve cardiac output representing a vital emergency measure to treat cardiac tamponade.

Public domain health.mil
Anatomy
The pericardium, representing an inverted cone shaped sac surrounding the heart, rests on the top of the diaphragm. It is made up of two layers:
An inner layer or visceral pericardium, made up of a single layer of mesothelial cells lining the pericardium. An outer layer, composed of dense fibrous tissue, also known as the parietal pericardium.
In relation to its location and neighboring structures, the pericardium in a parietal layer is attached at the bottom to the central tendon portion of the diaphragm.
In its upper portion this layer is joined to the sheath surrounding the large vessels. In the anterior part, attached to the posterior surface of the sternum, it is later joined to the spine, the esophagus, the bronchi and the aorta.
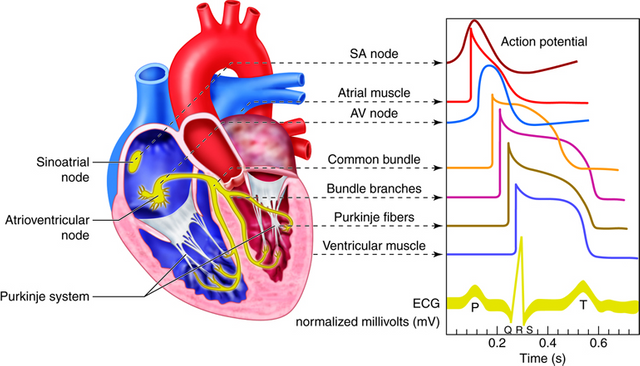
Anatomy of the Heart. Electricity line in heart. Author Rasel Hossain Md. Licensed CC BY-SA 4.0
The heart is located inside the pericardial sac, both the right and left ventricles, the atria, the aorta, the pulmonary artery and the inferior vena cava are closely related to the anterior thoracic wall and damage to it can cause severe cardiac complications. Therefore, injuries, generally traumatic at the anterior thoracic level, can trigger pericardial effusion and finally cardiac tamponade.
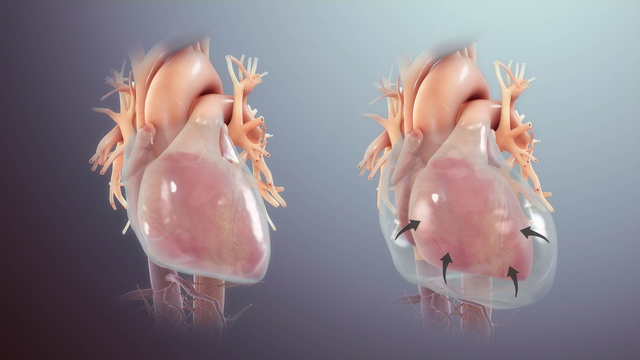
The pericardial cavity is a virtual space between the visceral and parietal layers of the pericardium. The presence of approximately 20 to 50 ml of fluid is normal; when it exceeds this limit we speak of effusion. When this limit is exceeded, we speak of an effusion. Since this fluid in normal quantities fulfills the function of lubrication during cardiac movement.
Cardiac Tamponade
Cardiac tamponade is a life-threatening situation that must be diagnosed and treated immediately. Its diagnosis is primarily clinical, especially those patients with a history of chest trauma. The symptomatology of this complex picture will be given by the accumulation of fluid under pressure in the pericardial space.
However, there are special situations where a chronic pericardial effusion of more than 1 liter to 2 liters is evident, which does not show signs of cardiac tamponade and is well tolerated by the patient. When this happens, we must suspect that it is secondary to a neoplastic process, whether diagnosed or not, a history of aortic section, acute myocardial infarction, or some drugs such as oral anticoagulants.
We must take into account that the presentation of cardiac tamponade can also be provided by iatrogenic causes, including central line placement, transthoracic cardiac pacemakers, transvenous and cardiopulmonary resuscitation.
Physiopathology
Physiologically, the organism in the initial stages of tamponade, tries to exercise compensatory measures, prior to the collapse, mediated by the release of catecholamines, increased systemic venous pressure, and compensatory tachycardia.
There comes a time when the capacity of the pericardial space to distend and accommodate is exceeded. When this happens, only small amounts of fluid in this space generate a great deal of pressure that impacts on the cardiac chambers; as this pressure increases, the venous filling of the heart decreases dramatically, thus, cardiac perfusion decreases and the heart suffers injuries.
When the accumulation of fluid in this space increases, the intrapericeric pressure increases, bringing as a consequence the decrease of the cardiac output.
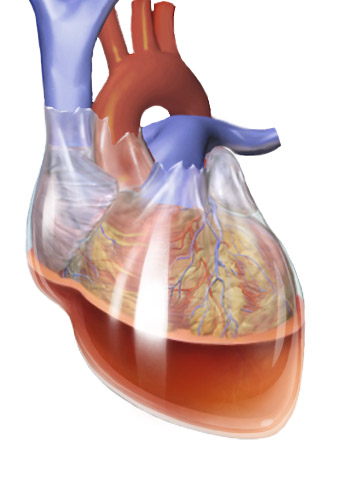
CC BY 3.0
Etiology
Clinical signs of cardiac tamponade
These symptoms may not be as florid, if the patient is suffering from signs of hypovolemia.
Beck's triad of muffled heart sounds, hypotension, and jugular venous ingurgitation is associated with cardiac tamponade.
Patients with cardiac tamponade will have at least one of these symptoms. It is usually accompanied by other symptoms such as psychomotor agitation, fatigue, dyspnea, tachycardia and tachypnea. This can progress to shock, coma and eventually death.
The paradoxical increase of the jugular venous pressure during inspiration and paradoxical pulse, can be evidenced in individuals that cure with this pathology.
The paradoxical pulse is nothing more than the drop in systolic pressure greater than or equal to 10 mmHg during inspiration.
It is frequent to observe in the ECG, changes in the morphology or amplitude of the QRS complex, which is a product of the heart swinging from one side to the other in the pericardial space occupied by liquid.
The presence of micro complexes is usually the most common in these cases.
The finding of an enlarged cardiac silhouette on chest X-ray may be useful in chronic pericardial effusion, but is considered a non-specific sign.

Pericardial effusion with tamponade CC BY-SA 3.0
Cardiac ultrasound, or echocardiogram, is the diagnostic procedure of choice in these cases. CT and MRI are diagnostic modalities that should only be used in stable patients, when a diagnosis is not established and there is a discrepancy with respect to the presence of pericardial effusion or cardiac tamponade.
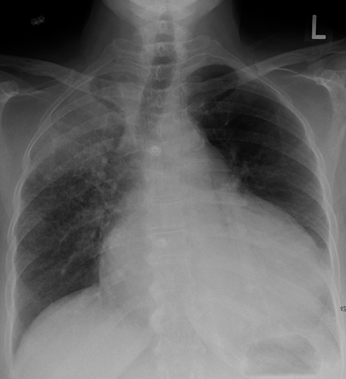
X-ray of Thorax. Cariomegalia Unspecific sign. CC BY-SA 3.0
Indications
The only urgent indication for pericardiocentesis would be in a patient where the physiological changes of cardiac tamponade are present and threaten the patient's life.
Contraindications
Severe bleeding disorders, in a medically stable patient this procedure is contraindicated. Patients with a history of trauma should initially have an aggressive replacement of crystalloid and concentrated fluids and a needle thoracotomy to release a tension pneumothorax before considering paracentesis.
Preparing the patient
Always explain to the patient and/or representative about the procedure to be performed.
Position the patient so that the heart is in contact with the anterior chest wall. Connect the patient to a heart monitor, pulse monitor, and supplemental oxygen. Place the noninvasive blood pressure monitor on the patient's arm.
Insert a nasogastric tube to decompress the stomach, as this will decrease the chance of perforating the gastric chamber during the procedure.

Public domain needpix
Identify the anatomical references needed to perform the procedure, the needle intended for the execution of this procedure, can be inserted in several places:
Below the xiphoid appendix, at the right or left sternocostal margin, (Subxyphaloid approach).
In the fifth intercostal space on the right or left parasternal space (parasternal approach).
In the fifth intercostal space with mid-clavicular line (apical approach).
Blind insertion technique
Trace the skin with a #11 scalpel needle between the xiphoid appendix and the left costal margin. Insert the spinal needle through the skin incision at a 45° angle in the mid-sagittal plane.
Direct the tip of the needle towards the patient's left shoulder or alternatively towards the right clavicle midline or sternal base, thus avoiding injury to the coronary arteries.
Advance the needle about 4 to 5 cm while exerting negative pressure, until blood returns through the syringe, revealing normal phonetic heart sounds or changes in the morphology of the QRS complex on the ECG.
If at any time the ECG shows changes suggestive of injury or damage to the myocardium, remove the needle at 1mm or 2mm intervals until the ECG pattern normalizes, as these changes are probably secondary to the syringe needle touching the myocardium.
When entering the pericardial space and aspirating the fluid, a marked improvement in the patient's clinical condition should be seen, and as much fluid should be withdrawn as possible. If the syringe is completely filled, the aspiration will be stopped and the syringe withdrawn, but by first securing the needle in position, the syringe is quickly replaced with a new one and the procedure continued.
Alternatively, a three-way wrench may be taken between the spinal needle and the syringe, connecting a third party to an intravenous extension tube. As much fluid as possible should be drawn in and out, and the needle should be gradually withdrawn.
Technique by ECG monitoring
The goal of ECG monitoring is to prevent accidental puncturing of the ventricle with spinal water.
As the spinal needle advances, a pattern of damage is observed that is characterized by an elevation of the ST segment, as long as this needle touches or penetrates the myocardium.
The presence of ventricular extrasystoles or a ventricular arrhythmia may also mean injury to the myocardium.
Prepare the patient as described above and connect him/her to the ECG, proceed to insert and advance the needle until it reaches the pericardial space. If changes suggestive of injury to the myocardium are present, proceed to withdraw the needle at least 1 0 2 mm, until the changes observed on the ECG disappear. Finally, aspirate and remove as much fluid as possible.
Seldinger technique
Useful in cases of pericardial effusion of medical or traumatic cause, since this technique allows us to save time, if we do not have a surgical room.
The technique is similar to taking a central venous line.
Clean and prepare the patient, insert the spinal needle, blind or with ECG monitoring. Take and secure the spinal needle with the non-dominant hand, gently withdraw the syringe from the spinal needle with the dominant hand.
Insert the guide through the needle into the pericardial cavity, approximately one third. Remove the needle over the guide while holding the guide in the pericardial cavity.
Insert the dilator while holding the guide, then carefully remove it while holding the guide in place.
Advance the catheter over the guidewire into the pericardial cavity and proceed to remove the guidewire and secure the catheter to the skin, finally connect a syringe to the catheter and aspirate the fluid from the pericardium, this should significantly improve the patient's clinical status.
Ultrasound-guided technique
It is currently considered the gold standard with respect to patient care, benefit and integrity. The point of needle insertion will be where the pericardial effusion is greatest.
The location and direction of the ultrasound waves should be monitored by the person performing the pericardiocentesis. The procedure is the same as the blind invasion or ECG monitoring technique, but in this case the progress of the needle can be visualised, redirected and drained more easily and with less risk of injuring neighbouring structures.
Ultrasound of human heart. CC BY-SA 3.0
Confirmation
We must bring note that the absence of blood extraction does not rule out the presence of cardiac tamponade, what happens in these false negatives, is that probably the fluid in this cavity, this coagulated and not allow the passage of the same through this needle so fine, usually happens in about 80% of cases.
The patient's blood pressure and cardiac output should improve as this fluid is extracted from the cavity and therefore this confirms the correct extraction.
It is advisable to perform a chest x-ray after the execution of the technique, in order to rule out a hemothorax or pneumothorax.
Complications
The rate of complications ranges from 4 to 40%, and it decreases in those procedures guided by ultrasound.
Death, bleeding or ventricular arrhythmias are the most feared complications.
Reaccumulation of fluid in the pericardial space occurs in 70% of cases executed blindly. Continuous drainage may decrease the frequency of this complication.
Bleeding, hemothorax or pneumothorax, may be secondary to injury from the spinal needle when introduced into the pericardial cavity and may injure arteries, veins and lungs. To minimize this risk, it is recommended that the needle not be rocked or changed in direction once inserted into the patient.
The presence of fibrillation, arrhythmias, ventricular tachycardia or asystole if the myocardium is injured.
Finally
In general, pericardiocentesis is an infrequent procedure that can be life-saving if the patient is in severe cardiac tamponade.
The procedure is simple, but has a high rate of morbidity and mortality complications.
The use of ECG and echocardiogram is essential for the diagnosis and treatment of the procedure, drastically avoiding false diagnosis and complications.
Sources:

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
If you have any questions about any topic of medicine or present any disease you can comment the publication or write me in discord and I will attend you.
Dr. Ana EstradaI hope you enjoyed my content.
Congratulations @anaestrada12! You have completed the following achievement on the Steem blockchain and have been rewarded with new badge(s) :
You can view your badges on your Steem Board and compare to others on the Steem Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPTo support your work, I also upvoted your post!
Your level lowered and you are now a Red Fish!
Congratulations @anaestrada12!
You raised your level and are now a Minnow!
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.