YELLOW FEVER
YELLOW FEVER
It is an acute viral disease transmitted by the bite of a mosquito, which must be previously infected. It is a virus belonging to the family Flaviviridae, genus Flavivirus.
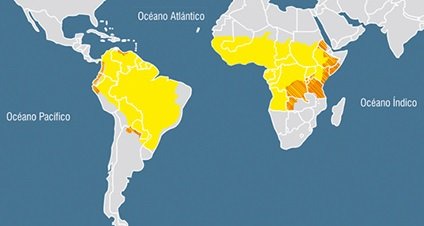
It occurs in tropical and subtropical areas of South America and Africa, it has NOT been described in Asia.
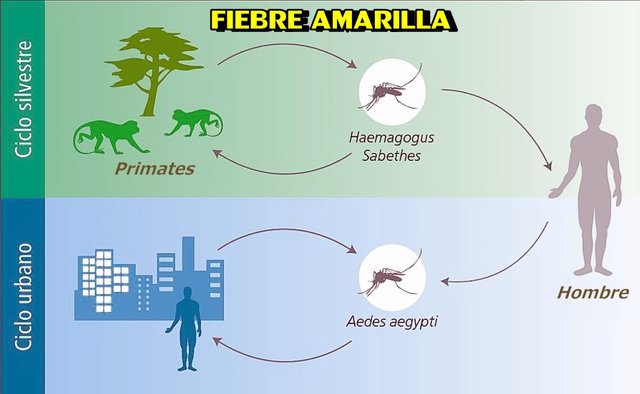
The virus will be transmitted from one host to another by the bite of a hematophagous arthropod. These vectors, when feeding on a viremic host, ingest the infecting virus and after a period of incubation in the insect, this is endowed with the capacity to transmit the disease to other animals or susceptible persons. Yellow fever is a zoonosis of the apes.
There are 2 transmission cycles: jungle and urban.
• • Jungle cycle: the virus circulates among primates, NOT in humans. The main vectors in America are mosquitoes of the genus Haemagogus (in Venezuela the most important vectors are: H. splendens, H. equinus, H. capricornae and H. leucocelaneus) and Sabethes, while in Africa they belong to the genus Aedes. In both continents, the reservoir is the monkey.
• • Urban cycle: circulation of the virus in susceptible humans. It is transmitted by the bite of the Aedes aegypti mosquito. This cycle begins when a person who has acquired the infection in the forest moves during the phase in which the virus circulates in their blood (viremia) to urban centers with high density of Aedes aegypti, where it is stung by said vector, which In turn, it will transmit the virus to another susceptible person, thus establishing the start of transmission in the urban environment.
Period of transmission: Few days before the onset of fever and during the initial 3-5 days of the disease.
In Venezuela there are 3 natural foci of yellow fever:
- The focus of Guayana: Located in the Bolívar state, among the populations included in this focus are Upata, El Palmar, Guasipati, El Callao, Tumeremo and El Dorado. Another focus of importance in this area is the Carona River.
- Focus of Lake Maracaibo: constituted by the jungle areas surrounding Lake Maracaibo and extending north and south to the foothills of the Andean mountain range of Trujillo, Mérida and Táchira states and west to the foothills of the Sierra de Perijá.
- The focus of San Camilo: It covers the Piedmont of Apure, Barinas, Mérida and Táchira states, in the basins of the Capara, Uribante, Nula and Sarare rivers.
PATHOGENESIS
After the inculcation period, a period of approximately 24 hours elapses during which the virus can not be detected, after this period of eclipse, the liver becomes the main target.
Between 72 - 96 hours:
• Necrotic and acidophilic changes are observed in the Kupffer cells, followed by changes in the hepatocytes (apoptosis) and the bodies of Councilman are produced.
• The mediozonal region of the hepatic lobule is affected and the cells in the vena cava are respected.
Between 96 - 120 hours: the changes reach their fullness.
• Numerous bodies of Councilman are found and the necrosis of the middle zone is accentuated.
• Intranuclear inclusions (Torres bodies) can be visualized.
• Marked adipose metamorphosis of the cytoplasm.
Liver damage is direct and inflammation is minimal.
In the Yellow Fever, a hemorrhagic diathesis is characteristic, due to the decrease of the synthesis and/or increase in the consumption of the coagulation factors.
Renal involvement is due to hypoperfusion and acute tubular necrosis, which generates proteinuria and renal failure. While encephalopathy may be due to cerebral edema, metabolic alterations, hypoperfusion or direct involvement by the virus.
CLINICAL MANIFESTATIONS
It can occur as a nonspecific febrile condition (abortive form) or with all the classic symptoms in the most severe cases. 1/20 presents a clinical picture with jaundice.
In forms with defined clinical manifestations, the incubation period lasts 3 - 7 days. The disease begins with the so-called "period of infection", followed by a "period of remission" and in 12-25% of cases after remission, the "period of intoxication" appears
- Period of infection (viraemic phase):
• Elevated fever - sudden onset
• Chill
• A headache
• Myalgia
• Low back pain
• Nausea
• Conjunctival injection
• Severe decay.
• Faget sign (slow pulse in relation to temperature)
- Remission period:
• Fever and most symptoms disappear.
• In the abortive form of the disease, it is normal for it to get here and it follows a rapid recovery.
- Period of intoxication (the virus is NOT present and antibodies appear):
In 12-25% of cases, after a remission of one or 2 days, this second clinical phase may appear. This is characterized by:
• Fever
• Abdominal pain
• Black or brown vomit, is classic.
• Jaundice (50% of the cases that present it are fatal)
• Hemorrhages (mainly in the skin, mucosa and digestive tract)
• Other important findings: oliguria, hypotension, and alt. of consciousness (delirium, stupor or coma)
In the terminal phase the patient can present:
• Shock
• Cheyne-Stokes breathing and hypothermia.
• Hypothermia
Weakness in convalescence can last for weeks.
Complications:
• Pneumonia
• Sepsis
• Late deaths, even weeks after having recovered from the acute disease and this is due to the development of myocardial damage, arrhythmias, renal failure.
• Suppurative mumps.
DIAGNOSIS
Laboratory findings: prognostic value
• Leukopenia (absolute neutropenia and lymphopenia)
• Thrombocytopenia
• Proteinuria
• Increase in urea, creatinine, and direct bilirubin.
• The increase of ALT - AST (> 1000) - It correlates directly with the severity. They rise during the 2nd and 3rd day, reach their maximum 2-5 days later and in patients who survive rapidly decline between 10 - 14 days.
• Prolongation of TP - TPT
• Decrease in factors II, V, VII, IX, and X
• ECG shows sinus bradycardia.
Serology:
ELISA test
• Detection of specific IgM or increase in total antibodies -IgM, hemagglutination inhibitory (HI), complement fixation (CF) or neutralizing (N) - antibodies in 2 samples (acute phase and convalescence).
or IgM, Hemagglutination inhibitors, and Neutralizers appear between 5 - 7 days
o FC between 7 - 14 days
Viral isolation: (First 5 days of fever)
By inoculation of mosquito cells and detection of viral antigen in infected cells by immunofluorescence.
TREATMENT
No existen antivirales efectivos para esta enfermedad.
Symptomatic
• Paracetamol (a headache and fever)
• Cimetidine or Ranitidine + antacids (↓ risk of gastrointestinal bleeding)
Supportive therapy
In the period of intoxication to help the patient survive, although not always effective.


Nice post.. Need more exposure? If you want get followers, upvote and resteem