Reconstructed the face of a 14 year old and gave him a new chance at life
The best feeling in the world has to be meeting a patient in the post-operative care room after being present throughout their life-saving surgery in the operating theater. I experienced this incredible feeling yesterday after spending over 24 hours on duty in the Maxillofacial Surgery department, where we deal with all sorts of challenging cases you can imagine.
From road traffic accident (RTA) victims with their faces severely injured, to cancer patients facing the worst prognoses, to those suffering from multiple facial fractures—it’s all part of our daily routine. Even cases as extreme as maggots in the mouth are not uncommon. Whatever you can imagine, we encounter it regularly.
Our team recently encountered a similar case, and as the junior-most member, I had the greatest opportunity to learn. I made sure to make the most of this chance and kept asking my senior surgeons countless questions every second. I asked so many, in fact, that a few of them seemed visibly annoyed. However, after the surgery, they reassured me that they appreciated my enthusiasm for learning.
We even had the head of the Maxillofacial Surgery department with us in the operating theater, which was quite intimidating, to be honest. Working under his watchful eye was both challenging and inspiring.
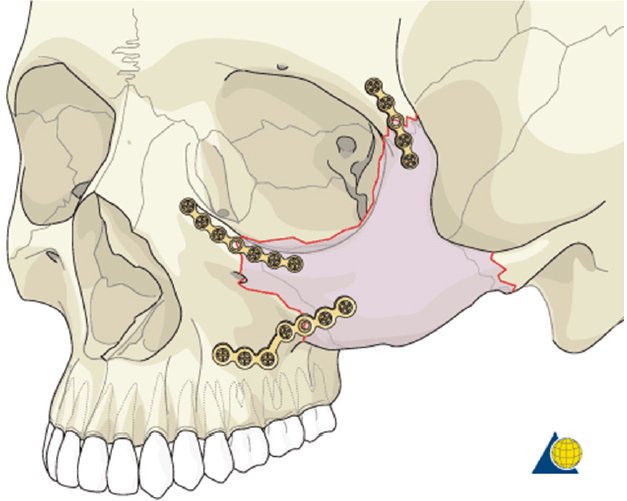
The patient we treated was a 14-year-old boy who had been in a bike accident, resulting in multiple facial fractures. These included a fracture of the body of the mandible, a zygomaticomaxillary complex fracture, and a small parasymphysis fracture.
Given the multiple fractures in his mandible, we had to adopt an exceptionally precise and effective approach to ensure the best outcome
The patient, obviously, was treated under general anesthesia and we had anesthesiologists with us on board. The surgery to be done was an ORIF which means open reduction and internal fixation.
A careful incision was made intraorally to gain access to the fracture site. With dissection, we exposed the fractured mandible while preserving surrounding vital structures like the mental nerve.
Next, we debrided the area, removing any debris or tissue interfering with bone healing. Using reduction forceps, we aligned the bone fragments anatomically, ensuring proper occlusion of the teeth. This step is crucial for restoring both function and aesthetics.
Once the alignment was confirmed, we selected titanium plates and screws suitable for the fracture’s location and severity. For the body fracture, a larger plate was used for stability, while a smaller plate was applied to the parasymphysis fracture. Holes were drilled into the bone, and screws were inserted to secure the plates firmly.
After verifying the fixation and ensuring stable occlusion, the incision was closed with absorbable sutures.
This was a rewarding feeling for me. The best feeling was to meet the same patient in the Ward later at night at around 2 am in the morning when I visited to check his vitals and saw him doing extremely well with all his vitals in check.
The very next morning we had a mouth cancer patient which indeed was the most difficult surgery I have ever been a part of. I will share that experience in a different blog.
Regards,
Dr Huzaifa Naveed





Curated by : @karianaporras
Thank you @karianaporras :))
Great job surgeons, this is not an easy thing. This is I guess between life and death.
It indeed is between life and death.