SEC S20W5 || Hemolytic Anemias - Module 5
Hello, fellow Steemians! I'm thrilled to join you in this week's hematology module focused on 'Hemolytic Anemias' as part of the Steemit Engagement Challenge by @dexsyluz and @aaliarubab. As a medical student passionate about exploring and also sharing medical knowledgge, I find discussing these topics incredibly fulfilling especially when we delve into thee conditions that affect so many lives globally. Hematology with its intricate connection to the immunology and majorly to pathology, continues to fascinate me. In this post, I'll walk you through the basics of hemolytic anemias, including their causes, diagnostic features, and treatment options. I also have a personal case experience from my time in the Pediatrics ward, which helped deepen my understanding of these disorders. Let's dive into the world of hemolysis together!
Hemolytic anemias are a group of disorders where red blood cells (RBCs) are destroyed prematurely,much earlier than their typical lifespan of 120 days. This rapid destruction, known as hemolysis, can occur due to intrinsic factors like. (This phenomenon also saves the african population from different species of malaria, Ill later tell the physiology behin it)
Membrane defects of the RBCs(Hereditary spherocytosis, Paroxysamal nopctural hemoglobinuria), Enzyme deficiencies (G6PD deficiency, Pyruvate kinase deficiency) or Hemoglbinopathies (Sickle cell and beta thalassemia) and it can be external factors such as infections, autoimmune reactions, or certain medications, microangiopathic and the macroangiopathic
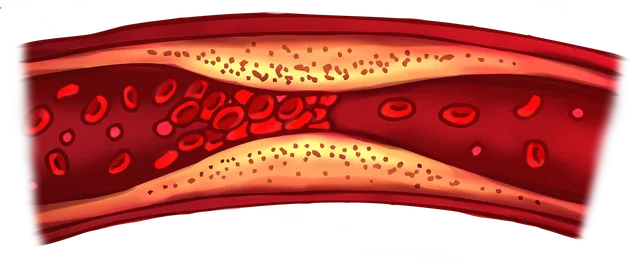
As the bone marrow tries to compensate for the loss by increasing the production of reticulocytes (immature red blood cells), it results in a high reticulocyte production index (RPI) of over 3%. This is why hemolytic anemias fall under the category of regenerative anemias, as the body is actively attempting to replace the destroyed cells. Symptoms of hemolytic anemias include fatigue, jaundice (due to elevated bilirubin levels), and sometimes an enlarged spleen and liver due to extramedullary hemotopoieses as already discussed in previous module
Sickle cell anemia is a hereditary genetic disorder (autosomal recessive, affecting both sexes equally) that alters the shape and functionality of red blood cells. The mutation affects the gene responsible for producing hemoglobin, leading to the formation of abnormal hemoglobin S. The mutation occurs in the beta-globin chain of hemoglobin. This causes RBCs to assume a sickle or crescent shape rather than the normal round form under unfavorable conditions such as hypoxia (low oxygen), acidosis (decreased pH), and dehydration (low fluid levels). These abnormally shaped cells are less flexible and often get trapped in small blood vessels, causing painful blockages known as vaso-occlusive crises. This can result in pain in the bones, abdomen, and chest, which may last for hours to days. The most common vaso-occlusive crises include Acute Chest Syndrome (ACS) in adults, which is the leading cause of death in sickle cell patients, and dactylitis (sickling in the fingers causing extreme pain and ischemia) in children.
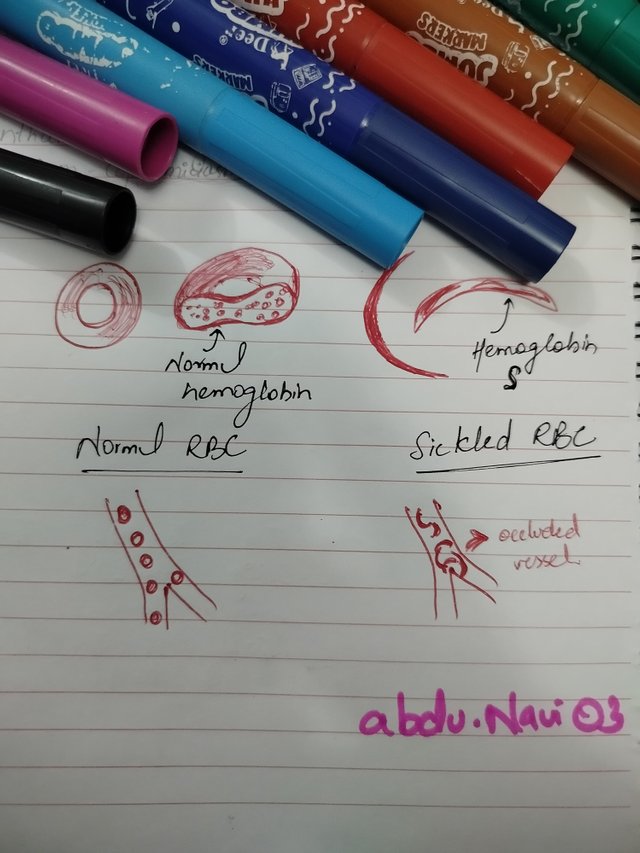 | 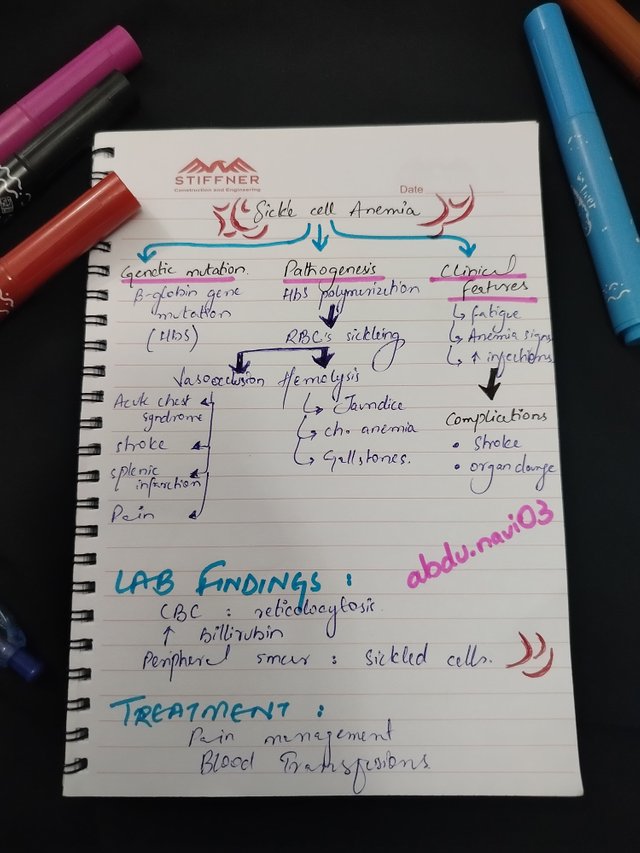 |
|---|
Due to their shape and rigidity, these sickle cells are more prone to breaking down, leading to chronic anemia (aplastic crisis). Sickle cell anemia is commonly found in individuals of African, Mediterranean, and Middle Eastern descent. Symptoms can include jaundice, gallstones, and enlargement of the spleen initially, and later in the disease, it can cause autosplenectomy (destruction of the spleen as constant obstruction due to sickling of RBCs irreversibly damages the spleen). Asplenia makes the body very prone to some encapsulated microorganisms, which is the main cause of death in children with sickle cell disease. Long-term, the repeated hemolysis can cause damage to the liver and other organs.
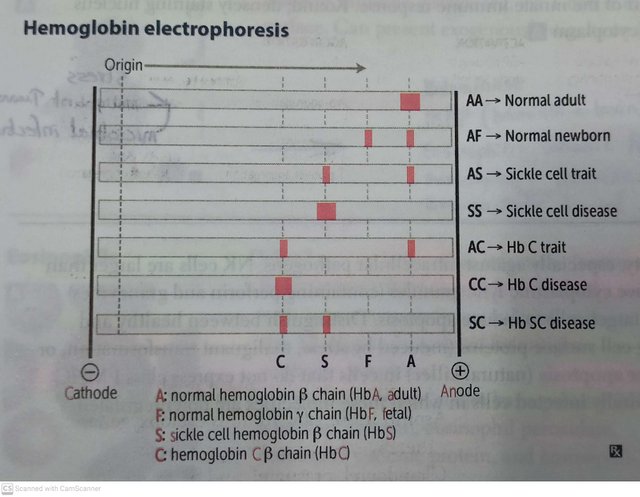
The diagnostic tests include the sickling test (in which metabisulfite is given to check if the cells sickle) and hemoglobin electrophoresis. Treatment often involves pain management, hydration, blood transfusions, and medications like hydroxyurea to minimize the frequency of crises.
| Feature | Intravascular Hemolysis | Extravascular Hemolysis |
|---|---|---|
| Definition | Destruction of red blood cells that occurs within the blood vessels, leading to direct release of RBCs content like hemoglobin directly into the bloodstream. | Destruction of RBCs occurs outside the blood vessels, like in the spleen or liver, by the help of macrophages (special immune cells). |
| Causes | Any mechanical trauma leading to vessel destruction, complement-mediated lysis (complements are proteins used against antigenic bodies, but if they auto-destroy our RBCs it can lead to hemolysis), toxins and infections. | It is usually caused by abnormal RBCs, (having an abnormal shape like in membrane defects or abnormal antigen like due to immune opsonization or beyond the age of >120 days) these abnormal RBCs are trapped and destroyed by macrophages in the spleen or liver. |
| Location | Intravascular (Intra=inside, vascular=vessels) occurs within the circulation (blood vessels). | Extravascular (Extra=outside, vascular=vessels) occurs in the spleen, liver, and sometimes bone marrow, where macrophages phagocytize RBCs. |
| Clinical Presentation | As RBCs are broken in blood, it can be seen as dark urine (hemoglobinuria), iron from RBCs in urine (hemosiderinuria), jaundice, and back pain due to hemolysis. | As the spleen and liver are overwhelmed, it can lead to an enlarged spleen (splenomegaly) and liver (hepatomegaly), yellowing of the skin (jaundice), anemia, and usually mild or no dark urine compared to intravascular hemolysis. |
| RBC Morphology | Fragmented RBCs on peripheral smear due to mechanical damage. | Spherocytes (sphere-shaped cells) can be seen due to incomplete phagocytosis of RBC membranes by macrophages. |
| Histology | Iron from destroyed RBCs (hemosiderin) can build up in the kidneys, and free hemoglobin may be floating in the bloodstream. | RBCs are seen inside macrophages in the spleen or liver, showing that the cells are being broken down by the body. |
| Example | Conditions where red blood cells break apart inside the blood vessels, like in PNH (a rare condition where red blood cells are more fragile), transfusion reactions (when the wrong blood type is given), mechanical heart valves (which can damage red blood cells), or malaria (a parasite that infects and destroys red blood cells). | Conditions where red blood cells are broken down mainly in the spleen, like in autoimmune hemolytic anemia (where the body attacks its own red blood cells), hereditary spherocytosis (a genetic condition causing fragile red blood cells), and sickle cell anemia (a condition where red blood cells become misshapen and break down easily). |
Back in June 2024, when I was posted in Pediatrics ward I got a similar case to witness. A 10-year-old boy was presented with complaints of continuous fatigue, intermittent episodes of fever and abdominal pain, progressive pale skin, and a recent history of jaundice (yellowing of the skin and eyes). According to parents he often gets tired easily while playing and has had recurrent episodes of dark brownish urine over the past few weeks. I thought it a simple case of anemia, but my senior doctor when did physical examination It changed my perspective of tackling such cases.
The senior doctor palpated enlarged spleen (usually spleen is not palpable), enlarged liver (>12cm), tender abdominal (painful abdomen) and suggestive signs of jaundice further narrowed down our diagnosis to hemolytic anemia. Lab investigations confirmed our diagnosis.
Lab Findings:
| Test | Patient’s Reports | Interpretation |
|---|---|---|
| Complete Blood Count (CBC) | Hemoglobin (8 g/dL), Elevated reticulocyte count, reduced mean corpuscular volume (MCV) | Indicative of anemia with active red blood cell turnover |
| Peripheral Blood Smear | Presence of spherocytes (abnormally shaped red blood cells) | Suggestive of extravascular hemolysis |
| Direct Antiglobulin Test (Coombs test) | Negative | No autoimmune hemolysis |
| Bilirubin Levels | Elevated indirect (unconjugated) bilirubin | Reflects increased breakdown of red blood cells |
| Lactate Dehydrogenase (LDH) | Elevated | Marker of cell destruction and hemolysis |
| Haptoglobin | Low | Indicates ongoing hemolysis |
Based on his clinical presentation, lab findings and mother’s history of such symptoms followed by splenectomy in her childhood, He was diagnosed with hereditary spherocytosis, which is so common in Pakistan. it’s a congenital form of hemolytic anemia. He was given supportive treatment for 2 weeks which included folic acid supplements, blood transfusion and ultimately gone through splenectomy in 3rd week. He’s now doing great in life, and I’m happy that he can now play without getting tired after 2 minutes.
To wrap up it in few lines, hemolytic anemias including conditions like sickle cell anemia and some others like hereditary spherocytosis, highlight the complexity and resilience of the human body. Understanding these disorders not only deepens our medical knowledge but also helps us develop empathy for the patients who face these challenges and their consequencess daily Whether it's through clinical experiences or sharing knowledge in forums like this every opportunity to learn and educate others plays a veryy crucial role in improving healthcsare outcomes. I hope this post has provided you with valuable insights into the world of hemolytic anemias. Feel free to ask questions or share your own experiences in the comments below—let's continue this learning journey together! Thank you for reading, and I look forward to your feedback and engagement.
regards,
Dr @abdu.navi03
Excellent work once again with your explanation of the anaemias specially the sickle cell anaemia