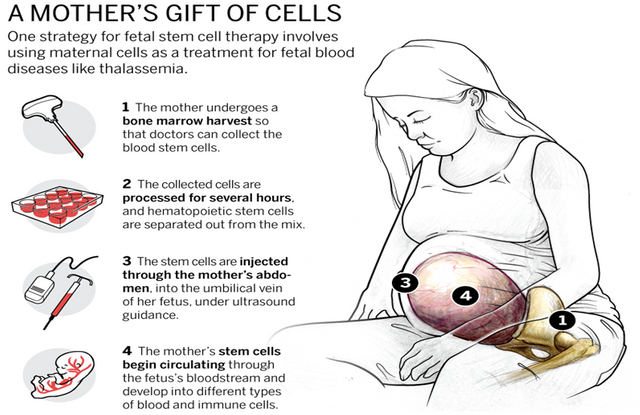
Mothers Cells

Source
Stem cells have great potential
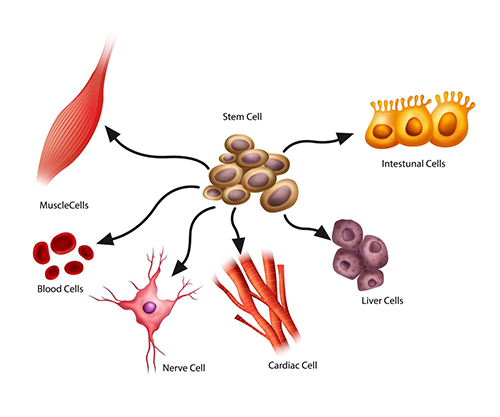
From the beginning, your cells do not know how they come together to form bone, heart or blood; they start as clean cells. These completely undifferentiated cells can be found during pregnancy, or when the baby is in the womb, and are known as embryonic stem cells. These early stage stem cells are master cells that have the potential to become any type of cell in the body.
There is great controversy surrounding the acquisition of embryonic stem cells and fortunately, we can also acquire stem cells that form just a little later, as is the case with umbilical cord tissue. These stem cells, known as adult stem cells, stay with us for a lifetime. (Later, we will learn why not all adult stem cells are the same.) Adult stem cells are more limited in the types of cells that can be converted, it is something known as specific tissues, but they share many of the same qualities . Hematopoietic stem cells (from the Greek "to make blood" and pronounced he-mah-toe-po-ee-tic) are found in the blood of the umbilical cord, for example, can become any of the different types of blood cells which are found in the body and are the basis of our immune system. Another example is the mesenchymal cells (meh-sen-ki-mal), which can be found in umbilical cord tissue and can become a large number of cells, including those found in the nervous system, organs of the cells senses, circulatory tissues, skin, stem medulla, cartilage, and much more.
Stem cells can reproduce / proliferate
In summary, we have certain types of stem cells that can be converted into a variety of different cells that are like men's rebirth of cells, but there is one more thing that makes special stem cells. This has to do with the way they duplicate themselves.
The body has two ways to create more cells. The first is usually taught in high school science. Known as cell division, which is where a cell doubles within its membrane before dividing into two identical cells. The cells do this, as needed for regeneration, which we are going to play in a second.
The other way that the body creates more cells is through its stem cells, and the stem cells do things a little differently. They undergo what is called asymmetric division, forming not one, but two daughter cells: one cell often duplicates an exact cell of itself, a new relatively clean stem cell, and another mother cell that is ready to become a specific type of cell. This characteristic is known as self-renewal and allows stem cells to proliferate, or reproduce rapidly.
Through these two means, we are always producing more cells. In fact, a large part of our body is in a state of constant renewal, because many cells can only live for a certain period of time. The lifespan of a cell in the lining of the stomach is about two days, and red blood cells, about four months. It is assumed that the nerve cells of the brain are supposed to live forever. For this reason, these cells rarely regenerate and would take a long time if they do.
Stem cells are regenerative
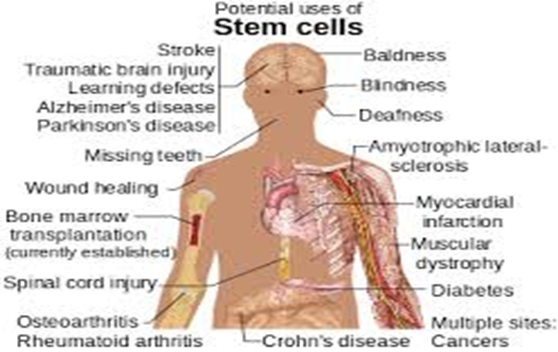
Stem cells are often obtained from the blood of the umbilical cord and the bone marrow. Different cells have different life cycles, and many are in constant regeneration, but when damage occurs and the body needs to go to a new supply of cells to heal itself, is dependent on the ability of stem cells to quickly create more cells to repair the wound. Here lies the potential for the introduction of new stem cells to improve or to be the driving factor in the healing process.
First, scientists found ways to use stem cells from bone marrow and following this discovery, the first stem cell transplant was performed in 1956 through the bone marrow between identical twins. Result was the complete remission of a twin's leukemia.
This and all other therapies with stem cells involve the introduction of new stem cells in the area to promote the healing process. Often, stem cells will create a particular type of cell, simply because it is in the proximity of other cells of that type. Unfortunately, researchers still have a long way to go before they can use the stem cells of unrelated people.
Source
Stem cells need to be compatible
The immune system has a way of identifying foreign cells; which is what allows the body to defend itself. So, although the transplants were giving good results after the first time in 1956, they were limited to twins because their shared genetic makeup made them 100 percent compatible. This took a turn in 1958, when scientists discovered a protein present on the surface of almost every cell that allows the body to know if the cell is one of its own cells or a foreign cell. In 1973, we finally learned enough about these compatibility markers (called human leukocyte antigens or HLAs) to perform the first unrelated bone marrow transplant.
The proteins come from three HLA genes, and inherit one HLA from each parent, or half from the HLA markers of their mother and the other half of their father. This gives the siblings a 25 percent chance of being a perfect match, a 50 percent chance of being partial match and another one out of four chance of not being absolutely compatible. Unfortunately, about seven out of 10 patients who need a transplant do not have a compatible donor in their family. They can either rely on their own stem cells, isolated before treatment or previously preserved, or try to find a compatible donor through a public donor.
A co-compatibility of HLA helps to ensure that the body accepts the new cell and that the transplant is successful. It also reduces the risk of graft-versus-host disease (GVHD), which is when the transplanted cells attack the recipient body. This disease occurs in 30% -40% of recipients when they are not a perfect match, but the donor is still related. If the donor and the recipient are not related, it increases to a 60% -80% risk. The better the compatibility, the more likely it is that the symptoms of GVHD are mild, in case you suffer from GVHD. Unfortunately, GVHD can also be deadly.
Source
Not all adult stem cells are the same
Other advances were made in 1978, when stem cells were discovered in umbilical cord blood and in 1988, when umbilical cord blood stem cells were used for the first time in a transplant. Stem cells taken from umbilical cord blood or tissue have already proven to be more advantageous than those taken from other sources such as the bone marrow. In many ways, this is because umbilical cord stem cells can be considered native and immature compared to stem cells from other sources. The umbilical cord stem cells have not been exposed to diseases or environmental contaminants, and are more receptive to foreign cells. In this case, lack of experience makes them stronger.
Here are some of the ways that cord blood stem cells are better than other stem cells:
The preserved cord blood stem cells are readily available when necessary.
Stem cells from the bone marrow require an invasive, surgical procedure.The preserved cord stem cells are more tolerant to tissue incompatibility and show a lower incidence of graft versus host disease (GVHD).
The preserved cord blood stem cells have a lower risk of transmissible viral infections.
The preserved cord stem cells have the ability to cross the blood-brain barrier, (between blood and brain) and can differentiate into neurons and other brain cells, which may be critical in the treatment of some brain disorders.
Stem cells have untapped potential
The use of hematopoietic stem cells, which can be found in the blood that remains in the vein of the umbilical cord and the placenta after birth, is a proven treatment in more than 80 diseases. Mesenchymal stem cells, which can be found in umbilical cord tissue and can become a large number of cells, including those found in the nervous system, sense organs, circulatory tissues, skin, bone, cartilage, and more, they are undergoing clinical trials and are promising in the treatment of stroke, heart disease, diabetes, autism, cerebral palsy and Alzheimer's disease.
