Antibiotics: even a low dose induces bacterial resistance!!
Hi steemians....
Thursday, February 1, 2018, a group of doctors spoke in Le Parisien to alert public opinion about the risk represented by overconsumption of antibiotics in France. Bacteria are resistant to the point of becoming sometimes multidrug-resistant, which complicates the treatment of many infections. In 2013, an article from the CNRS showed that even low doses of antibiotics can encourage resistance. These drugs should be used with the utmost economy.
A true therapeutic impasse, the emergence of multidrug-resistant bacteria is a phenomenon that makes the success of treatment of infections more and more random. This is particularly the case in hospitals, where multidrug-resistant bacteria are involved in nosocomial infections.
Whether in wastewater, or in people following antibiotic treatments, these environments may have a high bacterial concentration, with low amounts of antibiotics. Today, the physiological effects of these low concentrations of antibiotics on bacteria and the genetic events that may result are poorly understood.
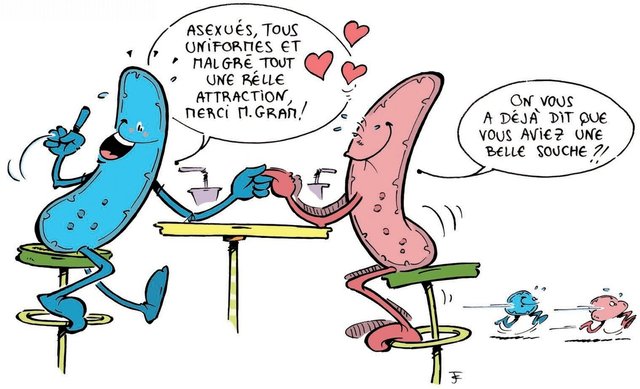
In Plos Genetics, researchers have shown that low concentrations of antibiotics belonging to the family of aminoglycosides (used in the hospital environment to treat many infections) favor the acquisition of resistance genes in several pathogenic bacteria, such as Vibrio cholerae (1). infectious agent of cholera), or Klebsiella pneumoniae (responsible for respiratory infections).
When the antibiotic bacterium screams SOS
Scientists explain this phenomenon through the following mechanism: antibiotic concentrations, even 100 times lower than the lethal concentration, trigger a stress response in the bacteria. Called "SOS response", it occurs when bacterial DNA is threatened, and promotes the acquisition of resistance genes by two routes. On the one hand, it causes an increase in the frequency of bacterial genome mutations. On the other hand, it activates a protein called integrase, whose role is to integrate or excise from the bacterial genome DNA sequences often carrying resistance genes, integrons.
In addition, the researchers also understood why in the presence of aminoglycosides, the SOS response did not take place in the Escherichia coli bacterium, whereas it is induced in other species that are very close genetically. The key to the mystery lies in the stabilization of the RpoS protein in Escherichia coli, which acts as a stress regulator in bacteria. In the presence of aminoglycosides, the researchers observed that RpoS prevents oxidative stress, which is responsible for inducing the SOS response in other bacteria.
In light of this work, induction of the SOS response appears to be an essential vector for the acquisition of new bacterial resistances. As a result, the factors and intermediates that lead to this response are potential targets for the development of new antibacterial therapies. The identification of the RpoS factor also suggests the development of possible adjuvants to antibiotics, in order to limit the impact of their effect at low concentration.
Source: https://www.pasteur.fr
Follow me @sparganose
Great research you did! We have to be very careful of what kind of antibiotics we use and how much of it. As you pointed out, even low doses are enough to cause an antibiotic resistance. It is also important to keep in mind that only in extreme cases we actually need antibiotics. In a normal, healthy human being the immune system is capable of killing the infection on its own. Nevertheless, many people tend to take antibiotics to become healthy sooner without considering potential side-effects.