The Gentleman Medical Series #1; Antibiotic Resistance Crisis

This is the first time in like ever I learned how to commit myself for hours in front of a computer, typing this article on my blog. Well, you have to sacrifice something to gain something, isn't it? I've learned something valuable, and at the same time, I'm satisfied with the outcome (my article). Now, let's talk about antibiotic. Antibiotic is one of the most popular therapeutic agents which are used for bacterial infections. As it is relatively easy for a clinician if all of the bacteria in the world are sensitive to an antibiotic, there are some which are persistent, which we called as the antibiotic-resistant bacteria. It is a common occurrence and has been one of the most critical topics in medical school.
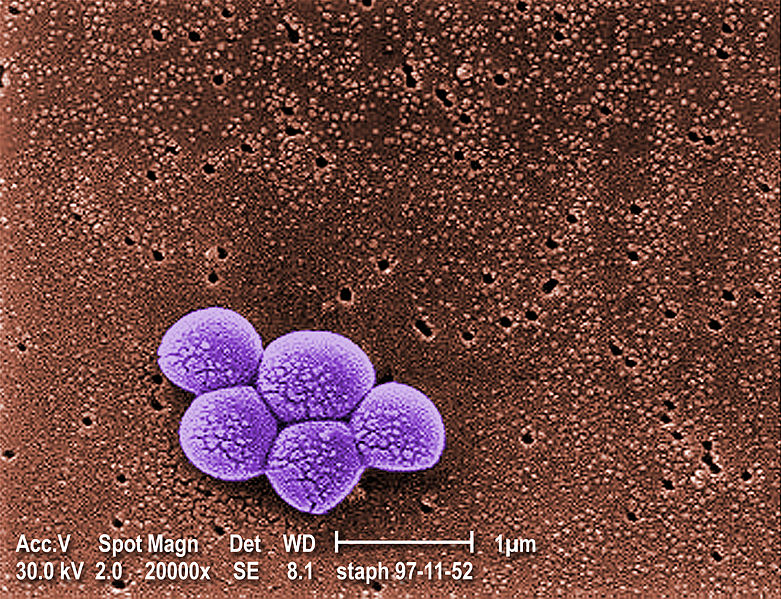
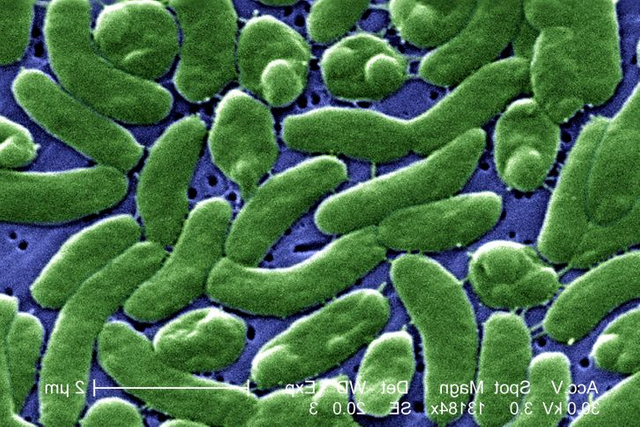
Methicillin-Resistant Staphylococcus Aureus (MRSA), Vancomycin-Intermediate Staphylococcus Aureus (VISA) and Antibiotic-Resistance Pseudomonas Aeroginosa; these are some of the badasses of nosocomial infection. For those who are not in the medical field, nosocomial infection is a hospital-acquired infection. Funny isn't it? People seem to think that hospitals are the cleanest place on earth. Oh boy, they are wrong.
When Alexander Fleming discovered antibiotic in 1928, he doesn't realise the potential of this particular agent to fight infection. Instead, he used it to treat superficial wounds and any infection on the surface of the skin. Well, it is understandable since antibiotic was discovered from a mould, I mean, who wants to eat that? It was not until 1940 when his colleagues demonstrated the capability of an antibiotic to act as a therapeutic agent, to treat various kind of infection caused by bacteria. Pretty neat, no?
Well, to be honest, there are only two ways how antibiotics were able to stop the bacteria from running amok. They either withhold them or kill them. Yeah, this is a cruel world, I know. If you want to know about it a little bit more detail because let's be honest, the answer that was given now is not entirely helpful; then I'll give you some more:
- They interfere with the bacterial DNA repair mechanism
- They deny the bacterial ability to produce new cells
- They destroy the integrity of the cell wall, making it weak and burst
Satisfied yet? I hope so. Well, most of the antibiotic prescribed when you first came to the hospital with a bacterial infection are classified under the broad spectrum antibiotic. As a medical student, this is like an answer scheme. Even if you space out a little bit, and doesn't know what the answer to the question given by your lecturer, sometimes, answering broad-spectrum antibiotic can be correct. Well, most of the time. Nevertheless, it would be relatively stupid to shout out antibiotic for cancer treatment, don't do that.
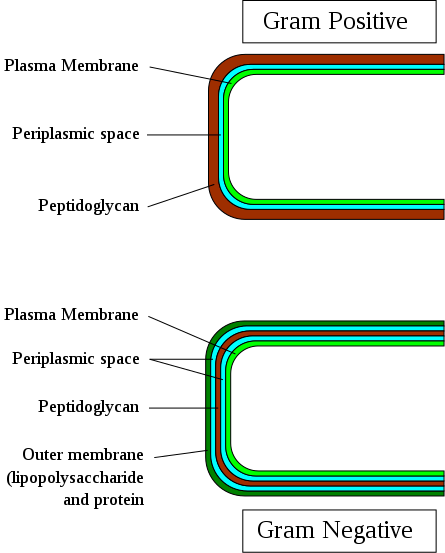
Broad-spectrum antibiotic works with a lot of bacterial infections regardless the type of cell wall that a bacteria have. Huh? What does that mean? Well, bacteria can be classified based on different morphological features, but when it comes to its cell wall, it can be categorised into two types:
- Gram-positive bacteria
- Gram-negative bacteria
There are a few structures which differentiate those two, but the things that matter is the peptidoglycan. I will cover this in the next episode of this series. Well maybe not after this, two to three episodes after this article. Anyway, if a broad-spectrum antibiotic failed to do its job or the microorganism which caused the infection has been identified, then, a special kind of antibiotic would be used. It is relatively more specific regarding its target, and it can only target one kind of bacteria (for example gram-positive bacteria only) but not both. It is called as the narrow-spectrum antibiotics (penicillins for instance).
Penicillin is a narrow spectrum antibiotic which is widely used in the clinical setting. To make it simple, it can destroy or inhibit the formation of cross-linkage between peptidoglycans which are essential to maintain the integrity of the cell wall. This phenomenon will cause bacteria to die as cell wall is relatively a crucial morphological structure for bacteria. Some antibiotics can block protein synthesis in bacteria by inhibiting the action of ribosomes which stunted its cell growth. These particular antibiotics are called, macrolide antibiotics; i.e. erythromycin.
Folate is an essential compound for bacteria to grow and multiply. It is synthesised in the bacteria by the action of an enzyme called dihydropteroate synthetase (DHPS). I know it's difficult to name to memorise, but this particular enzyme is critical as, without it, bacteria can't synthesise nucleic acids. A specific group of antibiotic which is called as sulfonamides can inhibit DHPS hence stunt the growth of a bacteria.
Antibiotic resistance crisis is one of the most serious problems that have to be dealt by medical practitioners all around the globe. These are some of the factors why antibiotic resistance developed among patients:
Antibiotic overuse: This particular phenomenon has been predicted by Alexander Fleming, five years after his colleagues had demonstrated the capabilities of these anti-microbial agents to fight off infection.
“public will demand [the drug and] … then will begin an era … of abuses.”
In some countries, antibiotics can be bought over the counter at the pharmacy, even without a prescription. This pattern of overuse among the general public has driven the development of resistance among bacteria species which is why treating infection becomes difficult from time to time.
"You got flu? Don't worry, take some of these antibiotics with meals."
Bad move. Despite all of the campaigns, awareness program and knowledge among the medical practitioners, antibiotics are continually being overprescribed around the globe. Well, sometimes, it is difficult to determine whether or not a patient needs an antibiotic or just some rest to heal. Prescribing antibiotic seems like the safest course of action, but it can cause undesirable consequences.
Incorrect Prescription: This is different from overused/overprescription. Assuming a doctor prescribed the correct antibiotic when it is not necessary, then it is an overprescription, but if the time is right but wrong antibiotics are given, then it is an incorrect prescription. Like an overprescription, an incorrect prescription of antibiotics can contribute to the bacterial resistance. A study which is conducted in 2014, by Luyt CE has found that, in 30-50% of an infection case, wrong antibiotics have been prescribed which could potentially cause complications from the side effects of the antibiotics.
An incorrect prescription can be regarding the type of antibiotics or the dosage given. Some people are prescribed with a low dosage of antibiotics which can result in strain diversification of a few species of bacteria such as Pseudomonas Aeruginosa.

Incomplete run of antibiotics: Nowadays, everyone is a doctor. Well, medical school is unnecessary because we have Google right? So why bother spending almost half a million of dollars to produce a single doctor? This attitude indirectly causes the emergence of resistance species when they decide to stop taking a specific course of antibiotic just because they feel fine. To put it simply, the antibiotics which are being manufactured to counteract the action of certain bacteria becomes less successful when that particular bacteria becomes tolerance.
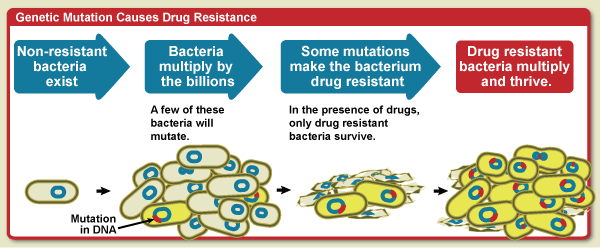
Some people might feel fine after finishing half of the antibiotics prescribed, but that doesn't mean that all of the pathogens has been wiped out. The remaining pathogens would mutate to survive; natural selection at its best. MRSA, VISA, some strain of resistant Pseudomonas Aeruginosa and Tuberculosis has become problematic due to people's ignorance of the importance of finishing the prescribed antibiotics.
Agricultural used: Most of the farmers in both of the developed and developing countries have been using antibiotics as a way to prevent livestock's infection thus improving livestock's general health. This is associated with a higher yield of high-quality product which could potentially increase their incomes. Continuous exposure could increase the number of resistant species among the bacteria. This particular resistant bacteria would be transferred to humans when we ingested improperly cooked meats. This phenomenon was identified 40 years ago when a study conducted yield an inexplicable result; some resistant strain of bacterial species has been found in the intestine of farmers and their livestock.
The event could be explained in the following sequence:
- The bacteria in the animal's intestine is being suppressed or killed by antibiotic leaving some resistant-form of those particular bacteria to emerge and thrive
- This resistant bacteria would be transferred to humans through food products, i.e. meats
- Humans experienced adverse health effect as the result of the action from this pathological resistant bacteria.
Antibiotic-resistant species of bacteria has been a threat to the medical communities since the dawn of time. This phenomenon is a global crisis. Medical doctors have been overprescribing patients with antibiotics; pharmaceutical companies have been selling antibiotics over the counter for maximum incomes; all of these factors signalled the need for a collaborative effort within the medical communities to minimise the incident of emerging antibiotic-resistant bacteria.
References
- Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40:277–283.
- Luyt CE, Brechot N, Trouillet JL, Chastre J. Antibiotic stewardship in the intensive care unit. Crit Care. 2014;18(5):480.
- Antibiotic Resistance Questions and Answers
- Antibiotic resistance
- About Antimicrobial Resistance
- Antibiotic Resistance: A Global Threat
- How do antibiotics work?
- Penicillin
- Antibiotic resistance



Nice job covering some of the main issues with antibiotic resistance. If you wanted to expand on this in future posts, I'd suggest looking into the development of new antibiotics (or lack thereof by pharma companies), or the ways in which horizontal gene transfer contributes to the spread of antibiotic resistance. Either way, glad to see some nice microbiology articles.
Hi @tking77798. Thank you for the suggestion. I'll make sure to remember that in the future.
I have seen that so many times... "I am feeling better, no need to finilize my treatment"... iiisshh.... :/
PS: great post by the way ^^
Sadly, that was true. Thank you @lemouth. Glad you like it.
Antibiotic resistant bacteria is a concern. I've changed some habits and activities to try to reduce my changes of infection. I did read about phage therapy. It's an alternative to antibiotics. Here's a paper on the topic if you're interested.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5547374/
Cool, I remember I saw one author wrote on this particular topic on Steemit. Not sure who.
Nice. I will have to search for it. Thanks for the heads up.
Hi @gameoverr. It seems that you are new here on Steemit. Welcome. Your article is great. Indeed antibiotic resistance has been a nuisance and always been a major global health problem. Keep on producing good content. If you have any problem regarding STEM-related articles, you can join steemSTEM Discord Channel and we will be glad to assist you.
Thank you @chloroform. Appreciate it.
Great Article, thanx a lot!!
I personally hope that a good alternative to antibiotics will be found. I am also sure that if medicine opens up to alternatives that are not just filling the wallet, this problem will be solved.
Greetings from Germany, Mo*
Hi @happy.food.life. That was a long name. Thank you for reading my article. Well, @epearson has attached a link to his comment about a potential replacement or substitution to antibiotic therapy called phage. Maybe you can refer to his comment to find out more about it.
You can say Mo* 😉
Yes, I already read it! Thank you!!
But I have to find some articles in German, its to hard for me to read in English! 😏😊
I see. Nice to meet you Mo*. :)
Welcome ;)
But I'd like to know something else. Do you really like to wear a suit and tie?
😉
Well, not really to be honest.
Then I'm reassured... Although, it can be sexy once in a while. Maybe you should think about it. 😂
Thank you for your wonderful and informative article regarding antibiotic resistance. Keep on producing quality material!
Thanks, @lordneroo. I will try my best to produce exciting articles in the future. Cheers.
Interesting one @gameoverr
well, these antibiotics resistant bacteria are real threat in present and that's the reason they are called superbugs, because they can modify their gene just in two three generation and can survive in the new antibiotic.
Cheers
Hi @vinamra. Yes, you're right, I've seen a few patients who have been infected with superbugs. The treatment modalities were quite complicated.
Interesting facts!! I might have to quit eating ground beef now. Can you write one of these articles about why doctors are giving out so many steroid shots? Resteemed
@c77hall, steroid shots? Care to elaborate?
Yes I don't know about in your area, but here in the southeast USA..they are giving steroid shots for everything from flu to poison ivy. I'm sure it's not the athletic steroids but its prednisone.
Hi, I just followed you :-)
Follow back and we can help each other succeed! #$
there are some countries with greater repercussions due to this inconvenience and among those we find those with scarce resources, the diseases abolished in advance spread in surprising ways and the antibiotics do not cause effects, since the infections are no longer the same