NIPAH VIRUS :- "a newly emerging zoonosis"
Hope you all are having a good time!!

image source by Ch1902 vector, Pepetps raster CCo3CCo2.5CCo2CCo1
Today we are going to discuss on a newly emerging zoonosis that causes severe disease in both animals and humans.Actually Zoonosis is an infection or disease that is transmissible from animal to humans under natural conditions.
Zoonoses can be caused by a range of disease pathogens including Viruses(HIV/AIDS, rabies, influenza, monkeypox, nipah virus disease, zika virus, ebola virus), Bacteria(clostridium difficile, bordetella bronchiseptica, erysipelothrix, rat bite fever, yersinia enterocolitica, anthrax, brucellosis), Fungi(cryptococcosis, dermatophytosis, histoplasmosis), Parasites(toxoplasmosis, leishmaniasis, cryptosporidiosis, cysticercosis), Arthropods(scabies), and Prions diseases.
Nipah virus
Nipah virus infection is a newly emerging zoonosis caused by Nipah virus which manifests as severe disease in both animals and humans.It can also be transmitted through contaminated foods or directly between humans.Nipah virus is a type of RNA virus in the genus Henipavirus.
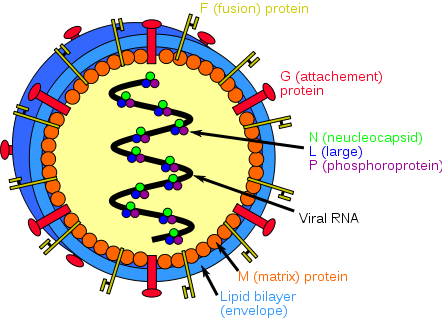
image source by Rhys at English Wikipedia CCo3
(Figure shows structure of Henipavirus)
Henipavirus is a genus of RNA viruses in the family Paramyxoviridae, order Mononegavirales containing five established species. Henipaviruses are naturally harboured by pteropid fruit bats (flying foxes) and microbats of several species.So the natural host of this virus is fruit bats of the Pteropodidae Family, Pteropus genus.

image source by Gregg Yan CCo3
(Fruit bats of the Pteropodidae family are the natural host of Nipah virus)
History and Epidemiology
Nipah virus was first identified during an outbreak of disease that took place in Kampung Sungai Nipah, Malaysia in 1998.On this occasion, pigs were the intermediate hosts. However, in subsequent Nipah virus outbreaks, there were no intermediate hosts.No new outbreaks have been reported in Malaysia since 1999.It was also recognized in Bangladesh in 2001, and nearly annual outbreaks have occurred in this country since then.
In Bangladesh in 2004, humans became infected with Nipah virus as a result of consuming date palm sap contaminated with bat saliva or urine with subsequent transmission to people.The disease has also been identified periodically in eastern India.Human-to-human transmission has also been documented, including in a hospital setting in India.During the later outbreaks in Bangladesh and India, Nipah virus spread directly from human-to-human through close contact with secretions and excretions of infected persons.From 2001 to 2008 all occurring between December and May, around half of reported cases in Bangladesh were due to human-to-human transmission through providing care to infected patients. A total of 135 human cases of Nipah infection in Bangladesh were recognized, of which 98 (73%) died.
One outbreak of Nipah Virus occurred in Siliguri, India, 15 kilometers north of the Bangladesh border in January and February 2001.The transmission of the virus was reported within a health-care setting, where 75% of cases(66 people) occurred among hospital staff or visitors and a second Nipah Virus outbreak was reported by newspapers in Nadia District, India, also close to the border with Bangladesh, in 2007.On 28th may the Hindustan Times reported the first suspected case of Nipah to be found outside the virus’s origin in the state of Kerala, in a young man who travelled by train to Goa. In Kerela, India, at present at least 40 people have been infected and 16 deaths have been recorded, including one healthcare worker. Those who have died are mainly from the districts of Kozhikode and Malappuram, including a 31-year-old nurse, who was treating patients infected with the virus. Till 31 May 2018, about 16 people have been quarantined because they had contact with the sick.
WHO reports Nipah Virus has mortality rates of up to 75%, though the recent strains to appear in India seem less deadly than that. A closely related virus called Hendra first appeared in Australian racehorses in the mid-nineties.
Other regions may be at risk for infection, as evidence of the virus has been found in the known natural reservoir (Pteropus bat species) and several other bat species in a number of countries, including Cambodia, Ghana, Indonesia, Madagascar, the Philippines, and Thailand.
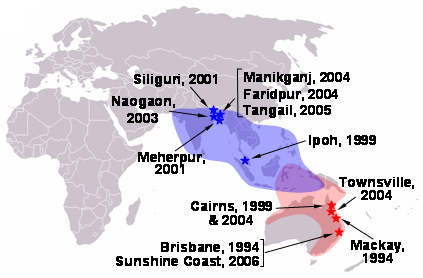
image source by Rhys at English Wikipedia CCo3
(Figure shows distribution of flying fox over the globe)
Transmission and clinical course
The recent outbreak shows, Nipah Virus can also be transmitted from humans to humans through bodily fluids, though the virus doesn’t currently have an airborne vector.The risk of exposure is high for hospital workers and caretakers of those infected with the virus. In Malaysia and Singapore, Nipah virus infection occurred in those with close contact to infected pigs. In Bangladesh and India, the disease has been linked to consumption of raw date palm sap and contact with fruit bats.
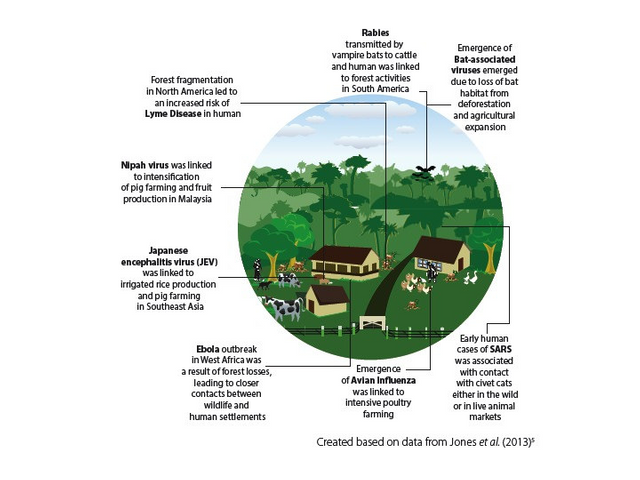
image source by Flickr CCo2
(Figure shows causes and transmission of zoonotic diseases)
Nipah Virus infection in humans has a range of clinical presentations, from asymptomatic infection to acute respiratory syndrome and fatal encephalitis.The clinical presentation of Nipah Virus infection in Bangladesh differed from Malaysia. In Bangladesh severe respiratory disease is more common, with 62% of cases having cough, 69% developing respiratory difficulty and available chest radiographs showing diffuse bilateral opacities covering the majority of the lung fields consistent with acute respiratory distress syndrome. By contrast, in Malaysia, 14% of patients had a non-productive cough on presentation; only 6% of chest radiographs were abnormal and these abnormalities were mild and focal.
source
In general initial symptoms are fever, headache, drowsiness followed by disorientation and mental confusion.Some people can also experience atypical pneumonia and severe respiratory problems, including acute respiratory distress. Encephalitis and seizures occur in severe cases, progressing to coma within 24 to 48 hours.Most people who survive acute encephalitis make a full recovery, but long term neurologic sequelae have been reported in survivors. Approximately 20% of patients are left with residual neurological consequences such as seizure disorder and personality changes. A small number of people who recover subsequently relapse or develop delayed onset encephalitis.
The symptoms start to appear within 3–14 days after exposure.However, an incubation period(interval from infection to the onset of symptoms) as long as 45 days has been reported.Respiratory illness can also be present during the early part of the illness.People with Nipah virus disease, who had breathing difficulty are more likely than those without respiratory illness to transmit the virus.The disease is suspected in symptomatic individuals in the context of an epidemic outbreak.
The case fatality rate is estimated at 40% to 75%. Highest case fatality rate of 73% has been reported from Bangladesh.In Malaysia, case fatality rate is only 39%.
Diagnosis
Initial signs and symptoms of Nipah virus infection are nonspecific, and the diagnosis is often not suspected at the time of presentation.This can hinder accurate diagnosis and creates challenges in outbreak detection as well as effective and timely infection control measures.In addition, the quality, quantity, timing of clinical sample collection and the time needed to transfer samples to the laboratory can affect the accuracy of laboratory results.
Laboratory diagnosis of a patient with a clinical history of Nipah Virus can be made during the acute and convalescent phases of the disease by using a combination of tests. Virus isolation attempts and real time polymerase chain reaction (RT-PCR) from throat and nasal swabs, cerebrospinal fluid, urine, and blood should be performed in the early stages of disease. Antibody detection by ELISA (IgG and IgM) can be used later on.Viral RNA can be isolated from the saliva of infected persons. In fatal cases, immunohistochemistry on tissues collected during autopsy may be the only way to confirm a diagnosis.
source
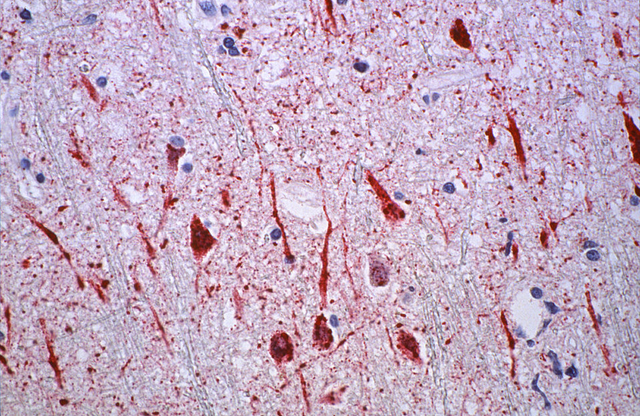
image source by CDC/ Brian W.J. Mahy, BSc, MA, PhD, ScD, DSc
(Above histopathological slide is from a human central nervous system tissue specimen affected by Nipah virus.It shows vasculitis with extensive thrombosis and parenchymal necrosis, endothelial cell damage, and syncytial giant cell formation in the vessels. Widespread presence of Nipah virus antigens in endothelial and smooth muscle cells of blood vessels are also seen)
Treatment
There is no vaccine for either humans or animals although WHO has identified Nipah virus infection as a priority disease for the WHO Research and Development Blueprint.The WHO states that a vaccine is being developed. The vaccine is a recombinant sub-unit formulation that has proven successful in cats. Canarypox vectored Nipah F and G vaccine has appeared promising for preventing infection in swine and also has potential as a vaccine for humans. A subunit vaccine, using the Hendra G protein, produces cross-protective antibodies against Hendra and Nipha virus and has been recently used in Australia to protect horses against Hendra virus. This vaccine offers great potential for henipavirus protection in humans as well. So at present the primary treatment for human cases is intensive supportive care.
Prevention
- Animal-to-human transmission prevention :-
Nipah virus infection can be prevented by avoiding exposure to sick pigs and bats in endemic areas and not drinking raw date palm sap.Eating of fruits partially consumed by bats and using water from wells infested by bats should be avoided.Domestic animals can also be the carriers of Nipah virus as fruit bats often drop partially eaten fruits which can be consumed by them. Try to keep them indoors and feed them yourself or if there's a chance of them being infected, keep distance from them and get them treated.Don't climb trees where bats may have left their saliva or secretions. - Human-to-human transmission prevention
Epidemiological surveys suggest that human-to-human transmission of Nipah virus is less common. The risk increases only when one gets in touch with the secretions of infected patients.The primary carriers of Nipah virus in humans are the respiratory secretions. If one encounters anyone who has the infection and has the chance to breathe in their exhaled air, one can get infected too. The risk gets very high if the patient has respiratory symptoms, such as coughing and sneezing. Because of the same reason, never share food, bed or be very close to a sneezing or coughing Nipah virus infected patient. At any cost, one should not come in contact with the saliva of an infected person.Regarding urine of infected person, a study published in the Journal of Infection, Nipah virus was isolated from the patients in the Malaysia outbreak and it was found that traces of Nipah virus were present in urine as well, besides saliva and throat swabs. So, one should be cautious while sharing washroom with an infected people.
Additional efforts focused on surveillance and awareness will help prevent future outbreaks. Research is needed to better understand the ecology of bats and Nipah virus. Surveillance tools should include reliable laboratory assays for early detection of disease in communities and livestock, and raising awareness of transmission and symptoms is important in reinforcing standard infection control practices to avoid human-to-human infections in hospital settings.

image source by Flickr CCo2
(Awarness programme on Nipah virus in Bangladesh)
References :-
1.http://www.who.int/csr/disease/nipah/en/
2.https://en.wikipedia.org/wiki/Nipah_virus_infection
3.http://www.who.int/news-room/fact-sheets/detail/nipah-virus
4.https://www.pastemagazine.com/articles/2018/05/the-nipah-virus-outbreak-everything-you-need-to-kn.html
5.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2784122/
6.https://www.cdc.gov/vhf/nipah/diagnosis/index.html
7.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1850894/
8.https://www.cdc.gov/vhf/nipah/prevention/index.html
THANK YOU!!
Steemstem
The Steemstem team has been working for over one year and now to promote informative S-Science T-Technology E-Engineering and M-Mathematics posts on steemit.The project aims is to build a community of Science and Technology lovers on steemit and aid in fostering the growth of posts and blogs.
To learn more about the project, you can join the channel in Discord here.
Hi @ameet77804.
If you have any problem regarding STEM-related articles, you can join steemSTEM Discord Channel and we will be glad to assist you.
Thank you @chloroform for your kind suggestions.I have corrected it.Please have a look and suggest more if I lack anything more to be corrected.Hope you will feel privileged to do it sir.
Thank you!!
Congratulations! This post has been upvoted from the communal account, @minnowsupport, by Amit from the Minnow Support Project. It's a witness project run by aggroed, ausbitbank, teamsteem, theprophet0, someguy123, neoxian, followbtcnews, and netuoso. The goal is to help Steemit grow by supporting Minnows. Please find us at the Peace, Abundance, and Liberty Network (PALnet) Discord Channel. It's a completely public and open space to all members of the Steemit community who voluntarily choose to be there.
If you would like to delegate to the Minnow Support Project you can do so by clicking on the following links: 50SP, 100SP, 250SP, 500SP, 1000SP, 5000SP.
Be sure to leave at least 50SP undelegated on your account.
Congratulations @ameet77804! You received a personal award!
Happy Birthday! - You are on the Steem blockchain for 1 year!
Click here to view your Board