Eptopic Pregnancy.
Medical Ultrasound Clinical Practice 2
CSN034
Case Report 2
Ectopic Pregnancy
Word Count: 2,200
Abbreviations:
RIF - Right Iliac Fossa EDD - Estimated Due Date
LNMP - Last Normal Menstrual Period IUP - Intrauterine Pregnancy
TAS - Transabdominal Sonography FHR - Foetal Heart Rate
TVS - Transvaginal Sonography IVF - In Vitro Fertilisation
IUCD - Intrauterine Contraceptive Device PID - Pelvic Inflammatory Disease
CRL - Crown to Rump Length FOV - Field of View
D&C - Dilation and Curettage POD - Pouch of Douglas
EP - Ectopic Pregnancy GS - Gestational Sac
G - Gravidity P - Parity
bHCG - Beta Human Chorionic
Gonadotropin
Title:
Right interstitial ectopic pregnancy during the 1st trimester.
Introduction:
This report has investigated a right interstitial EP, the aetiology, signs and symptoms, role of ultrasound and sonographic findings have being discussed. An EP is a complication in pregnancy where by the zygote implants itself within a region anywhere outside of the endometrial lining of the uterus and continues to develop. [1] It is considered a medical emergency however an interstitial EP carries the highest risk of mortality of all EP types due to the potential risk of hypovolemic shock when the fallopian tube in which it is situated ruptures. [5] It is responsible for approximately 10% of maternal deaths within the United States. [1,2] Fortunately the mortality rate has decreased from 1.15 deaths per 100,000 EP in 1980-1984 to 0.50 per 100,000 EP in 2003-2007. [8] The decrease in mortality is most likely traced to improved early detection rates by medical ultrasound, bHCG blood markers and increased public awareness of EP. [1,2] Sonography remains the primary tool for evaluating a 1st trimester pregnancy for confirmation of an IUP. [2]
Case Description
A 30-year-old female with G2 and P1 presented with increasing RIF pains for 1 week and a positive bHCG blood test of 2000 mIU/ml confirming that she is pregnant. The G. P’s physical examination also concluded that the RIF pain increased upon palpation. The LNMP from the G. P’s referral estimated that the patient is currently 8 weeks and 6 days gestation. The patient was referred for a 1st trimester dating scan for confirmation of a viable IUP and to acquire an accurate EDD for the duration of the pregnancy. The patient had no prior history of suffering from an EP, had nil complications with the first pregnancy and is otherwise healthy.
The LNMP dates and personal details were inputted into the ultrasound machine which corresponded with that of the GP’s referral (8 weeks and 6 days gestation). The exam commenced by utilising the C1-5 MHz TA probe. The patient was prepared with a distended bladder for the efficient propagation of high frequency soundwaves through the bladder which acts as an acoustic window to increase the clarity of the uterus, cervix and ovaries situated posteriorly. A full scan throughout the uterus from the left to right margins in a “sweeping” motion in longitudinal plane commenced. The same scan was commenced now in the transverse plane scanning through the superior fundus inferiorly towards the internal os. Multiple images were acquired during the scan of the uterus in both planes which concluded that no GS or IUP was currently present, it is also noted that the uterus is anatomically retroverted and that no pathology such as free fluid was located in the POD.
(just an idea, maybe put this part elsewhere when you’re talking about the
actual scan because you’ve gone from blood markers to GPs physical exam to ultrasound
machine to patient referral. It just doesn’t seem in ordeThe ultrasound machine used was the GE Logiq S8 initially starting the examination with the curved array TA C1-5D probe operating with a bandwidth of 1-5MHz. TVS was used as a secondary follow up scan using a TV IC5-9D probe with a bandwidth of 5-9MHz. Obstetrics 1st trimester mode was selected throughout the duration of the scan with consistent sonographer interactions with the ultrasound machine in reference to frequency adjustment, depth, TGC, focal point and overall gain to achieve optimal sonographic images.
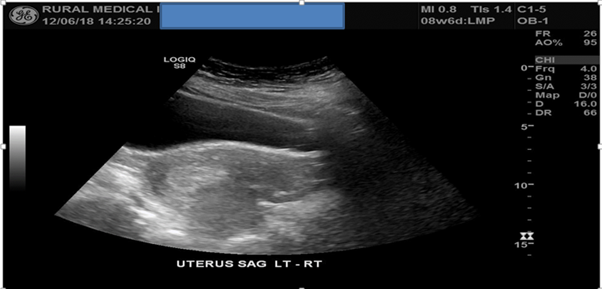
Figure 1: TAS of the uterus in both longitudinal and transverse planes failed to detect a GS or IUP.
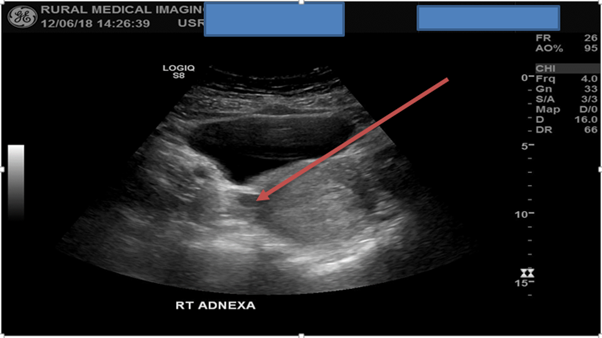
A scan of the left adnexa in the transverse plane from inferior to superior concluded that no pathology was detected but failed to observe the left ovary. A second sweep now of the right adnexa observed a well-defined anechoic lesion near the interstitial fallopian tube region. A possible GS was suspected, no obvious yolk sac or foetal pole was detected within the lesion. Literature states that the risk of an EP can exceed 90% when there is no detectible IUP and there is a corresponding adnexal lesion present. [1]
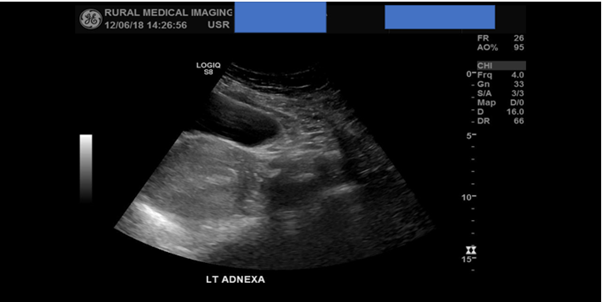
Figure 2: TAS of the left adnexa concluded no obvious pathology detected but failed to detect the left ovary.
Figure 3: TAS detects a well-defined anechoic lesion observed near the right interstitial fallopian tube region, highly suspected of being an EP.
In keeping with 1st trimester dating scan protocols TVS was offered to the patient. The procedure of TVS was fully explained by way of the sonographer stating to the patient that a long thin ultrasound probe with a sterile condom and lube applied will be placed into the patient’s vagina. The importance of TVS was explained that its closer proximity to the pelvic organs will result in much improved image quality and clarity as opposed to TAS which is subjected to attenuation from abdominal adipose tissue and air artefacts. [3] Patient’s verbal consent was granted prior to TVS occurring with words to effect of “yes you can continue” and “I understand the importance of the procedure”. The patient emptied their bladder and a female chaperone was present within the examination room throughout the scan.
TVS was started with the uterus in the longitudinal plane and the same “sweeping” scan method consistent with that of TAS was used. Also included in the scan was an assessment of the cervix in both longitudinal and transverse planes which found it to be of normal appearance. TVS detected an irregular shaped anechoic collection of fluid within the intrauterine cavity measuring 20x6x18mm with a volume of 1.12ml. This fluid was not detected using TAS, again no obvious GS or IUP was detected.
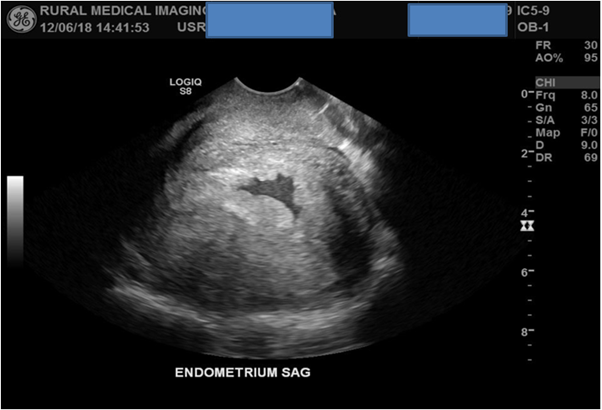
Figure 4: TVS detects an irregular shaped collection of anechoic fluid within the intrauterine cavity.
A superior scan in transverse plane of the right adnexa confirms the presence of a single GS with a possible internal foetus present. Although the initial first image was of suboptimal quality the HD zoom function was utilised for the next images for improved image optimisation and for confirmation of a possible live foetus. The angle of the TV probe was moved more inferiorly to place the pathology into the centre of the screen improving the FOV.
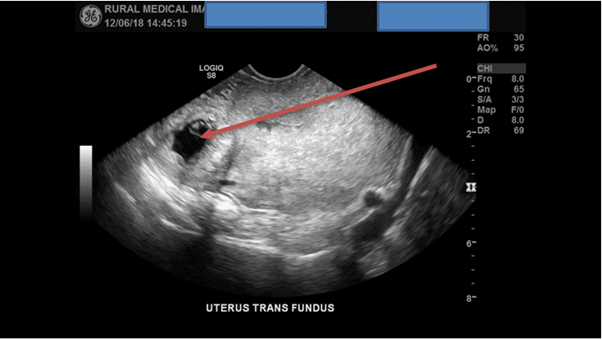
Figure 5: Initial images of a GS with a possible internal foetus are of suboptimal quality.
With the HD zoom function now enabled and an improved FOV multiple images of diagnostic quality were now acquired which confirmed that a right interstitial single EP was present. Three CRL’s were acquired totalling an average length of 7mm.
Further investigations revealed a normal appearing yolk sac measuring 1.3mm. M – Mode was utilised which found no detectible FHR present concluding that this foetus is deceased and has stopped developing.
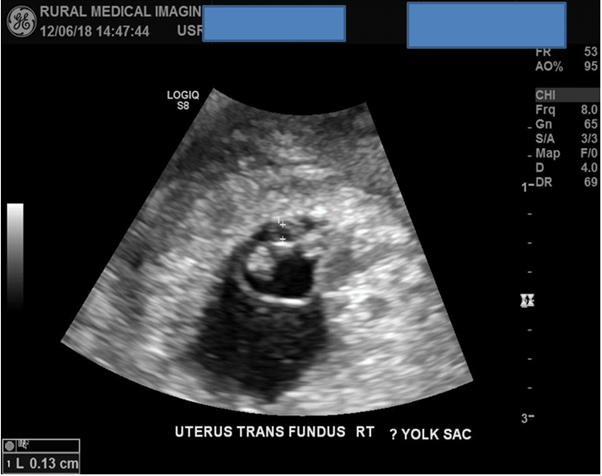
Figure 7: A yolk sac present measuring 1.3mm.
Figure 8: M-Mode initiated found no detectible 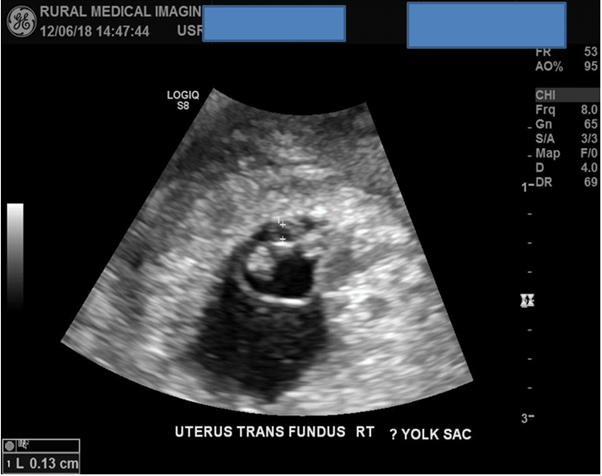 FHR, (Foetal demise).
FHR, (Foetal demise).
The scan processed with optimal images of the right ovary showing it to be of normal appearance with a volume of 5.4cc. Further images of the left adnexa were acquired concluding that no further pathology was present, but again TVS failed to visualise the left ovary.
Figure 9: The right ovary of normal appearance.
Figure 10: Calculations package, concluding the patient is 6w and 5d gestation.
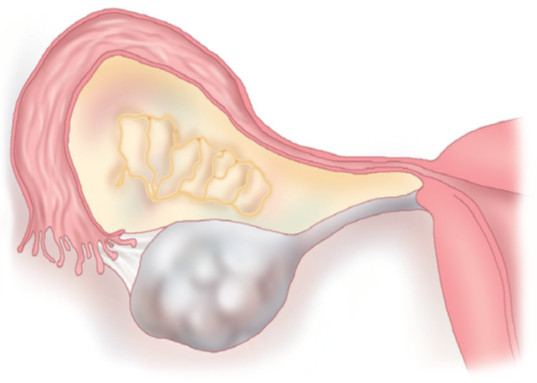
Figure 11: Anatomical diagram of the right fallopian tube. 97% of EP occur within the fallopian tubes. Source: https://www.kenhub.com/en/library/anatomy/fallopian-tubes
Discussion
An EP can present from many different aetiologies and present in many different ways dictated by its location of implantation. Current literature and evidence can place females into certain risk categories such as previously experiencing an EP, currently have an IUCD in-situ, females undergoing IVF, females administering ovulation inducing medications, previous fallopian tube surgeries and females who have undergone caesarean operations. [1] The vast majority of EP (97%) occur within the fallopian tube. [1] For this case in particular ultrasound confirmed the case to be an interstitial EP (fallopian tube ectopic).
The patient presented with increasing RIF tenderness, increased upon palpation and the knowledge that she was currently in her 1st trimester. Pelvic pain is one of the classic symptoms of an EP and has been reported in 97% of confirmed cases, although pelvic pain maybe consistent with other pathologies such as PID, endometriosis or UTI. [1] Other typical presenting signs and symptoms of EP included vaginal bleeding, abdominal pains, lower back pains, and amenorrhea however not all females will present with these classic symptoms and some can be asymptotic. [1]
The EP describe within this case is that of an interstitial EP. It is given its name due to its location at the junction of the fundus and fallopian tubes, it is thought to occur because of the small diameter within the fallopian tubes [1, 2] An interstitial EP is potentially the most life threatening of all of EP due to its location of implantation within the segment of the fallopian tube that enters the uterus. This segment is highly vascular where hypovolemic shock will occur if or when the EP ruptures out of the fallopian tube. [1]
TAS concluded the absence of an IUP and the presence of a right adnexal lesion. Follow up TVS first detected the presence of free fluid within the intrauterine cavity. Literature states that fluid within the intrauterine cavity is a soft sonographic marker of an EP. [7] One of ultrasounds main roles is to confirm the presences of an IUP and foetal viability. If a GS is detected containing no foetal pole then the chances of an EP is low however a follow up ultrasound scan and repeated bHCG blood tests should always be recommended. Examination of the bilateral adnexa’s using TAS is part of the scanning protocol with literature stating that EP can occur up to 25% of the time within the adnexa’s. [1]
TAS and TVS are different scans and so they possess different capabilities. They are normally used in conjunction (TAS used first) however if an EP is suspected TVS should always be offered. TVS greatly enhances image resolution of pelvic structures over that of TAS, although TVS possesses a lower FOV than TAS it has led to much earlier detections rates of EP. TAS used alone can detect approximately 10% of EP cases. [1] The improved image clarity of TVS allows for the exact location of a detected EP and the ability to detect a FHR and measurement of the CRL. [1]
bHCG is a hormone detected within the female’s blood and urine produced by the syncytiotrophoblast cells. It is needed to support the pregnancy by way of maintaining the corpus luteum in early pregnancy. [5] bHCG levels are directly related to the duration of the pregnancy which normally doubles every 2 days. A bHCG level of 1,800 to 2,000 mIU/ml is termed within the literature as the “discriminatory zone”. This discriminatory zone is used to differentiate between a normal IUP and an EP during ultrasound screening. For example, during ultrasound screening if no IUP or GS has been detected using TAS or TVS and the bHCG levels are within this discriminatory zone then there is a possibility of an EP. [1] If bHCG levels continue to rise post ultrasound screening then the possibility of an EP increases and follow up ultrasound screening is highly recommended. [1] Older literature indicates that a foetal pole can be detected on TVS with a bHCG level of 1,000 mIU/mL, however due to advances in ultrasound technology the imaging capabilities of TVS have been improved. Recent literature now indicates that a foetal pole can be detected with a bHCG level as low as 390 mIU/mL [5]. EP have been shown to demonstrate a lower than normal bHCG level as opposed to a normal IUP, however alternative literature puts this statement into controversy as it has also been shown that an EP can produce normal amounts of detectible bHCG when compared to that of a normal IUP. [1,2,5,6]
Conclusion
TAS and TVS when used in conjunction have shown their ability to diagnose a right interstitial EP with no detectible FHR. Although TAS was not able to directly detect the EP it did conclude that there was no IUP or GS present and the sonographer had prior knowledge that the patient was currently pregnant with bHCG blood markers of 2000 mIU/ml. With this prior knowledge of bHGC markers and no IUP or GS present the sonographer had advanced warning that a possible EP was present. TAS further proved its ability by detecting the lesion in the right adnexa. Follow up TVS was able to directly confirm this lesion to be a right interstitial EP. The foetus was clearly deceased and the GA from the LNMP was not concordant with that of the CRL. Although this foetus is deceased all EP should be classified as clinically urgent and effort should be made to contact the patients GP. The risk of fallopian tube rupture in this case is low due to the foetuses suspended growth (deceased). [4] However emergency transport (Ambulance) should be considered for transportation of the patient to hospital for possible right salpingectomy, D&C or ultrasound guided injection of Methotrexate. [4]